Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Usual interstitial pneumonia associated with idiopathic pulmonary fibrosis (IPF-UIP) has a poor prognosis with a median survival of 3 years. It is unknown whether myositis-associated UIP (MA-UIP) has an improved survival compared to IPF-UIP patients (pts). Our objective was to compare the cumulative and pulmonary event-free survival between MA-UIP and IPF-UIP.
Methods: Adult MA-UIP and IPF-UIP pts were identified using prospective registries. Pts with myositis (PM/DM/overlap) or the antisynthetase syndrome and radiographic UIP on HRCT scan (verified by a thoracic radiologist) or a lung biopsy revealing UIP histology were included. IPF pts met ATS criteria and had UIP pathology. Death status and date were verified with the Social Security Death Index. Kaplan-Meier survival curves and the log rank test compared cumulative and pulmonary event free survival (event = transplant or death) between a) all MA-UIP and IPF-UIP pts, b) MA-UIP pts with biopsy proven UIP (n=25) vs. IPF-UIP pts matched for age, gender and baseline FVC (±10%). Cox proportional hazards ratios compared overall and event free survival controlling for co-variates.
Results:
IPF-UIP pts (n=81) had a mean age of 63 (±8.4), 73% male, 98% Caucasian, baseline FVC% 65 (±15.3) and DLCO% 47 (±17.3). The MA-UIP patients (n=43) had a mean age of 46 (±11.0), 35% male, 83% Caucasian, baseline FVC% 60 (±19.6) and DLCO% 47 (±18.3).
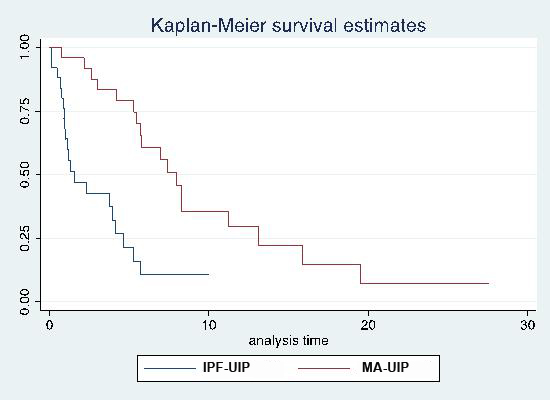
Median cumulative and event free survival time from diagnosis in IPF vs. MA-UIP was 5.2/1.8 years vs. 16.1/10.8 years, respectively. The 5 and 10 year % unadjusted event-free (graph 1) and cumulative survival was significantly worse in IPF-UIP vs. MA-UIP (25/0 vs. 80/50 and 59/32 vs. 80/65) (p < 0.001). The hazard ratio (HR) of IPF-UIP vs. MA-UIP pts was 2.86 (95% CI 1.45-5.61) for cumulative and 5.0 (95% CI 2.8-8.7) (p<0.001) for event-free survival. IPF-UIP event-free survival (but NOT cumulative survival) remained significantly worse than MA-UIP with a HR of 6.4 (95% CI 3.0-13.8) after controlling for age at ILD diagnosis, gender and baseline FVC%.
Out of 81 IPF-UIP, 36 died (mean age 68) and 45 had transplant (mean age 65) compared to 16 deaths (mean age 54) and 10 transplants (mean age of 54) in 43 MA-UIP. Respiratory failure was the most common cause of death in both groups, followed by infection.
25 biopsy-proven MA-UIP pts showed significantly better event free survival compared to matched IPF-UIP pts.
Conclusion:
MA-UIP pts demonstrated a significant survival advantage over a matched IPF cohort, suggesting that despite similar histologic and radiographic findings at presentation, the prognosis of MA-UIP is superior to that of IPF-UIP. Thus, in pts with a radiographic or pathologic UIP picture, it is critical to distinguish those with an underlying autoimmune etiology as their course and response to therapies may differ from pts with true IPF.
Graph1: Kaplan-Meier curve for event free survival of MA-UIP and IPF-UIP
Disclosure:
C. McBurney,
None;
R. Aggarwal,
None;
K. Gibson,
Consultant: Boehringer-Ingelheim biomarker program,
5;
K. Lindell,
None;
C. Fuhrman,
None;
D. Koontz,
None;
F. Schneider,
None;
N. Kaminski,
None;
C. V. Oddis,
Genetech Advisory Board,
6.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/myositis-associated-usual-interstitial-pneumonia-has-better-survival-than-idiopathic-pulmonary-fibrosis/