Session Information
Date: Friday, November 6, 2020
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Despite optimal medical therapy, joint space disease and skeletal damage persists in a subset of patients with PsA, many of whom requiring musculoskeletal (MSK) surgery for disease related morbidity. The purpose of this study was to determine the prevalence of MSK surgery in PsA patients, describe the type/indications for surgery and associated risk factors that increase the likelihood of undergoing MSK surgery.
Methods: A longitudinal single center cohort was analyzed to identify PsA patients who had MSK surgery from January 1973 to December 2019 inclusive. All cohort patients fulfilled the 2006 CASPAR criteria. Data from all MSK surgeries were collected using a web-based database. Patient charts were reviewed to confirm individual surgeries were MSK related and attributable to PsA by cross-referencing to clinical records and pre and post-operative diagnoses. Descriptive statistics determined the prevalence of MSK surgeries attributable to PsA, in addition to categories, indications and anatomical locations for surgery. A cox proportional-hazards model determined predictors at initial clinic visit for undergoing first MSK surgery. Lastly, a cox proportional-hazards model using time-dependent covariates evaluated the cumulative effect of PsA disease burden on undergoing MSK surgery. All models were adjusted for sex, age and duration of PsA at baseline.
Results: Of the 1574 patients in the cohort, 185 patients had 379 MSK surgeries related to PsA (Table 1). Common surgeries were arthrodesis (27%) and arthroplasty (27%). Common anatomical locations included the knee (28%) and finger (21%) with surgical indications representing deformities (42%) and inflammation/synovitis (42%). 59% of surgeries were joint sacrificing while 41% were joint retaining. Complete covariate data for the cox proportional-hazards model at initial clinic visit and the time-dependent covariate cox proportional-hazards model was present in 97 and 90 patients respectively. At baseline visit, higher age (hazard ratio, 1.043; p< 0.001) and total damaged joints (hazard ratio 1.047, p< 0.001) were predictors for undergoing first MSK surgery (Table 2). In time-dependent covariate analysis, biologic use (hazard ratio 2.890, p< 0.001), nonsteroidal anti-inflammatory drug (NSAID) use (hazard ratio 2.623, p< 0.001), the presence of nail lesions (hazard ratio 2.482, p< 0.001), higher age at baseline visit (hazard ratio 1.073, p< 0.001) and higher total actively inflamed joint count (hazard ratio 1.032, p< 0.002) were predictors for undergoing first MSK surgery (Table 3).
Conclusion: 11.8% of patients in our cohort had at least one MSK surgery attributable to PsA, with most surgeries being joint sacrificing in nature (59%). Older age at presentation and more severe disease evidenced by damaged joints at presentation, active inflammation, nail lesions and use of biologic therapy were associated with a higher risk of MSK surgery. Despite medical therapy, a significant number of patients still require surgical intervention for mainly deformities (42%) or inflammation/synovitis (42%).
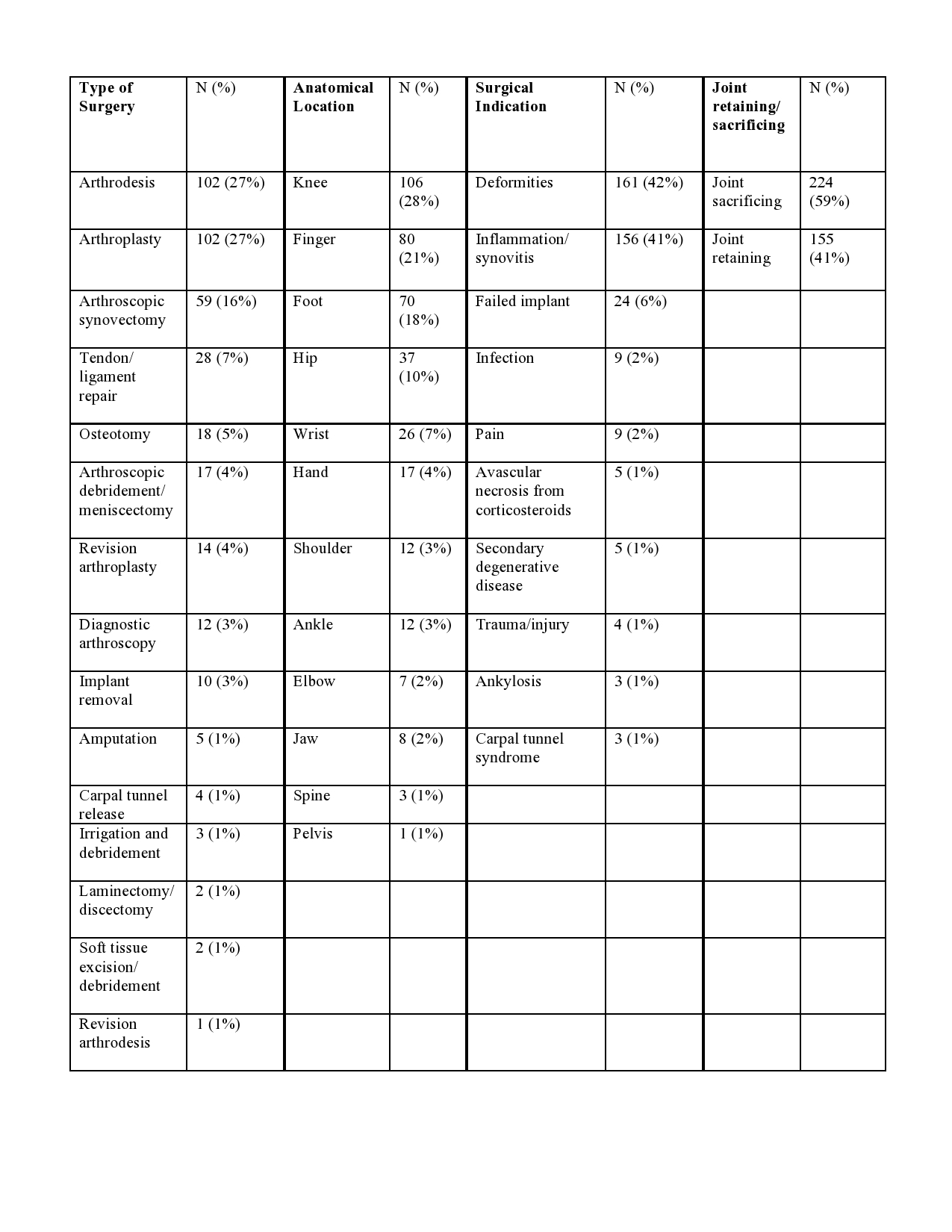 Table 1. Distribution and descriptions of MSK surgeries performed attributable to PsA (n=379)
Table 1. Distribution and descriptions of MSK surgeries performed attributable to PsA (n=379)
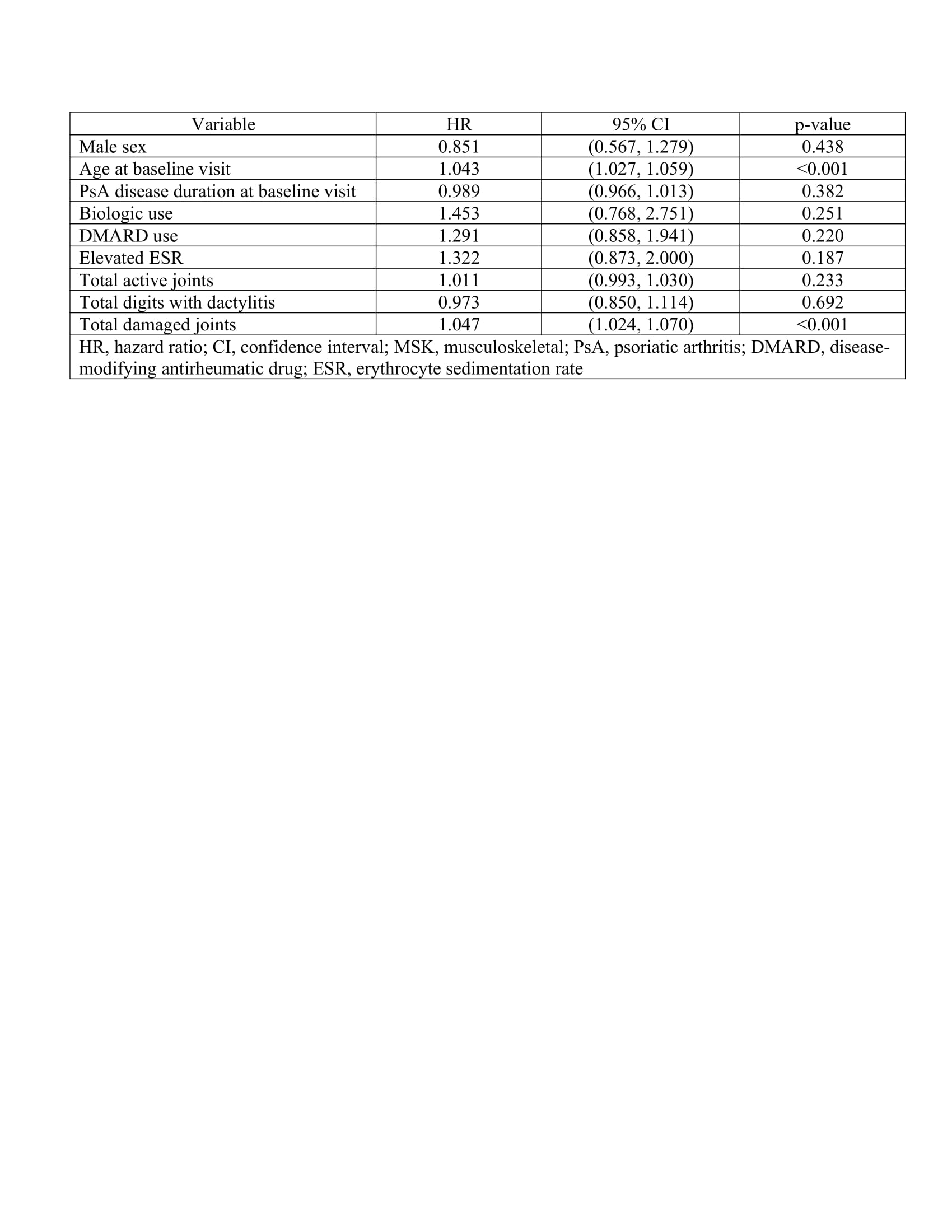 Table 2: Multivariate cox proportional-hazards model for predictors at initial clinic visit of undergoing first MSK surgery adjusted for sex, age and duration of PsA at baseline
Table 2: Multivariate cox proportional-hazards model for predictors at initial clinic visit of undergoing first MSK surgery adjusted for sex, age and duration of PsA at baseline
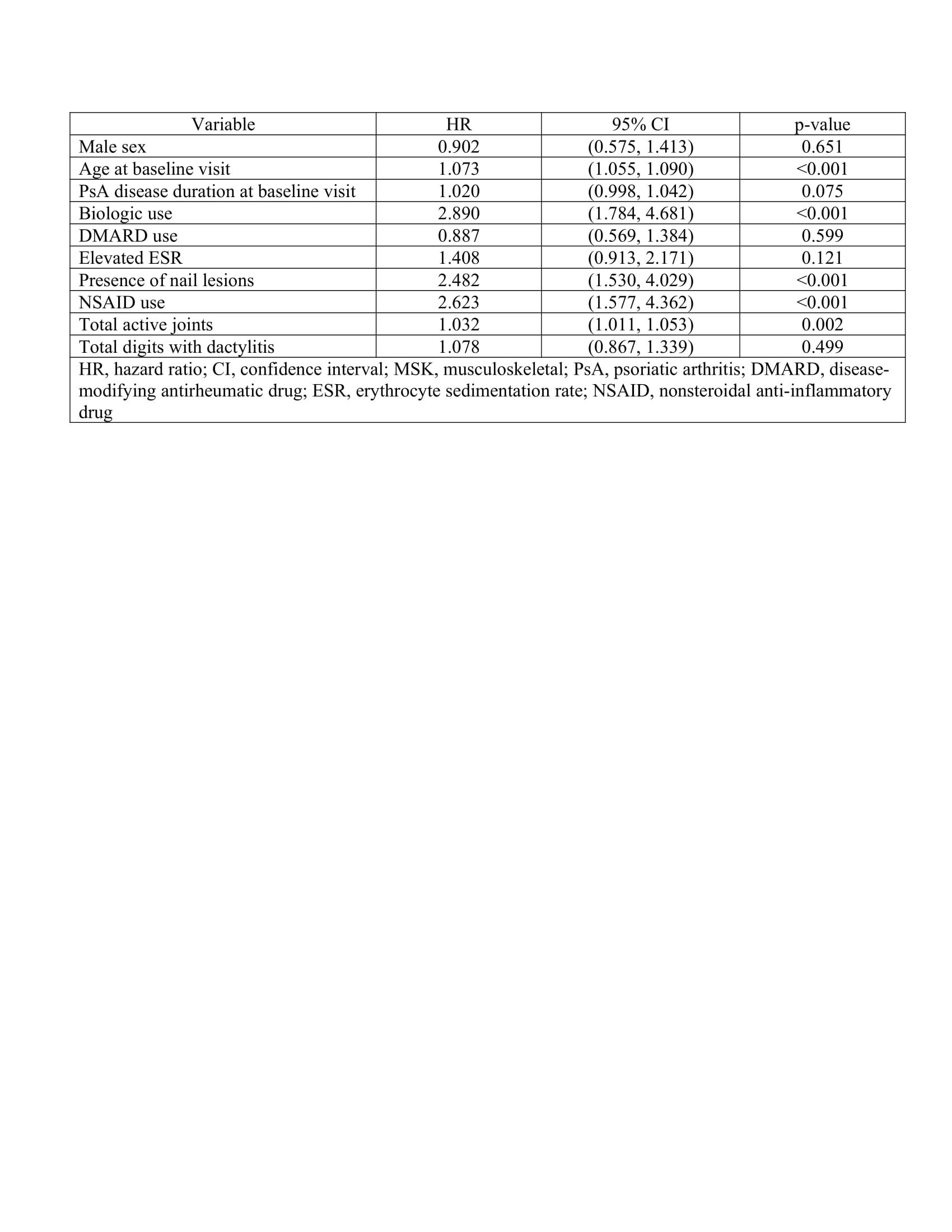 Table 3: Multivariate cox proportional-hazards model using time-dependent covariates for predictors of undergoing first MSK surgery adjusted for sex, age and duration of PsA at baseline
Table 3: Multivariate cox proportional-hazards model using time-dependent covariates for predictors of undergoing first MSK surgery adjusted for sex, age and duration of PsA at baseline
To cite this abstract in AMA style:
Kwok T, Sutton M, Pereira D, Chandran V, Gladman D. Musculoskeletal Surgery in Psoriatic Arthritis: Prevalence and Risk Factors [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/musculoskeletal-surgery-in-psoriatic-arthritis-prevalence-and-risk-factors/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/musculoskeletal-surgery-in-psoriatic-arthritis-prevalence-and-risk-factors/
