Session Information
Date: Wednesday, October 24, 2018
Title: 6W019 ACR Abstract: Measures of Healthcare Quality II: QI in SLE, Gout & JIA (2958–2963)
Session Type: ACR Concurrent Abstract Session
Session Time: 11:00AM-12:30PM
Background/Purpose: Lupus nephritis (LN), seen in up to 60% of individuals with SLE, progresses to end stage renal failure in 10-30% of patients within 15 years of diagnosis. Few studies have evaluated performance on LN quality measures. Using measures from the SLE quality indicators project and 2012 ACR guidelines for monitoring and treating LN, we evaluated quality of care for LN across multiple clinical sites for patients enrolled in the multi-ethnic, population-based cohort of the California Lupus Epidemiology Study (CLUES).
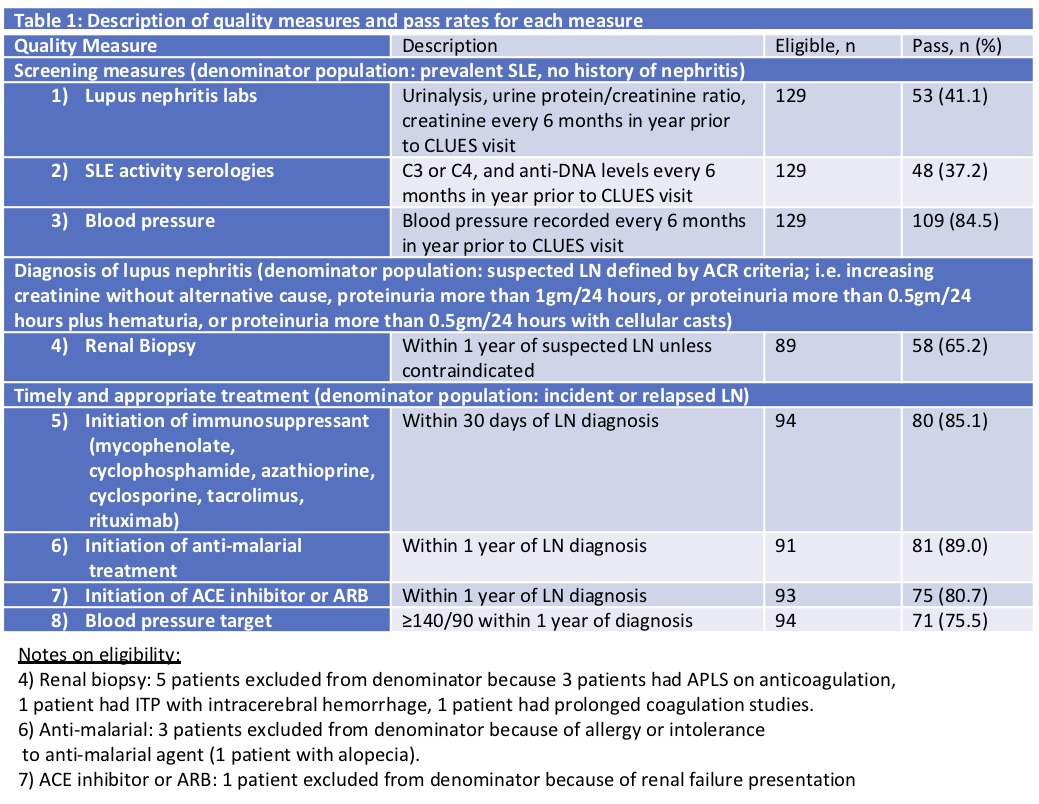
Methods: Participants were recruited from 2015 to 2017. Data were collected during in-person clinical study visits and from a comprehensive medical record review. The primary outcome was performance on LN screening measures in those without prevalent LN, and for diagnosis and treatment measures in those with LN (Table 1). Covariates were sociodemographics (age, gender, race/ethnicity, education, household income), clinical measures (disease duration and lupus severity index), and practice characteristics (provider setting and number of years with current provider). An overall pass rate was calculated, defined as the percentage of measures passed for which a patient was eligible; that is, among those eligible for a specific intervention, what percentage received it. Generalized estimating equations (GEE) with a logit function were used to estimate the probability of passing any one measure, with and without adjustment for covariates.
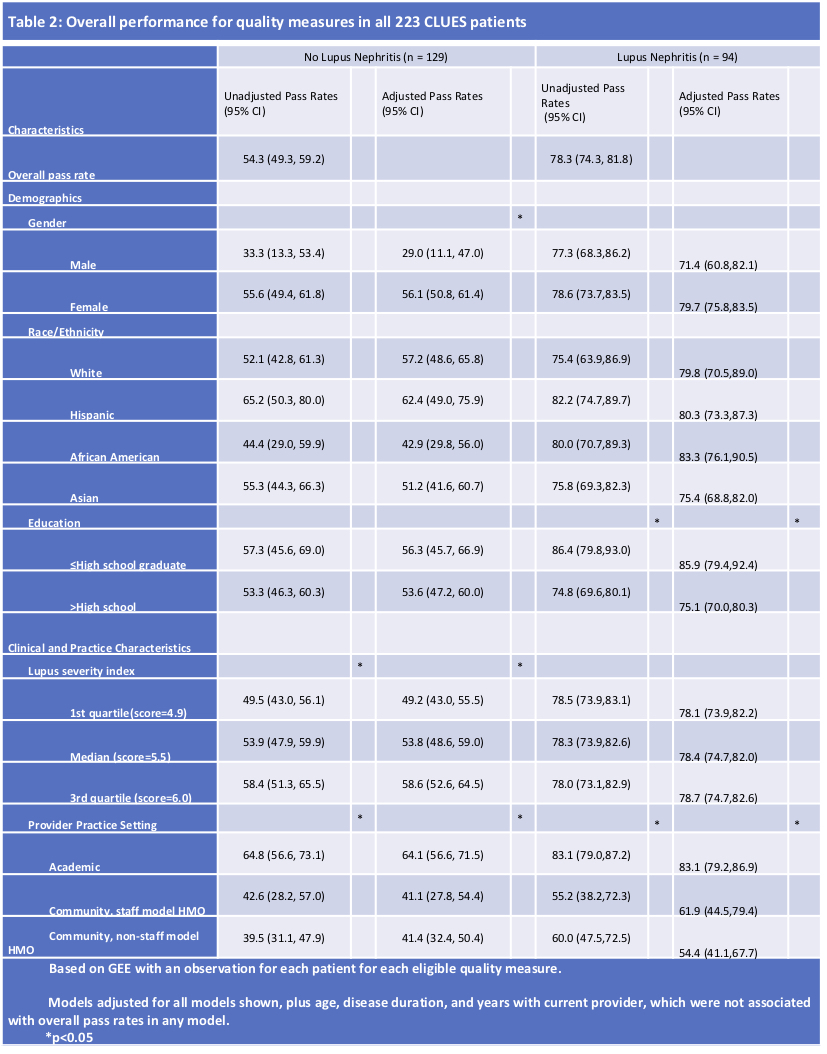
Results: Patients were followed in 25 clinical sites (2 academic, 1 staff model HMO with 6 practices and 17 community rheumatology practices). Performance on quality measures for 223 patients was evaluated, 94 of whom had LN. Overall pass rates were 54.4% for patients without LN and 78.3% for those with LN (Table 2). After adjustment in patients without LN, women and those with a higher lupus severity index had significantly higher pass rates, as did patients seen in academic settings. In patients with LN, patients with less educational attainment and those cared for in academic settings had significantly higher performance.
Conclusion: Across 25 diverse health settings, the largest gaps in care were for LN screening measures, with lower performance in community settings (vs academic) and for men. Across settings, performance was higher and more consistent for LN treatment quality measures, suggesting that once patients develop kidney disease, care is more standardized. Identification of these gaps in care can be used to target LN quality improvement initiatives.
To cite this abstract in AMA style:
Aggarwal I, Trupin L, Li J, Gaynon L, Liu N, Schlechter C, Murphy L, Dall'Era M, Yazdany J. Multi-Site Study Evaluating Performance on Lupus Nephritis Quality Measures [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/multi-site-study-evaluating-performance-on-lupus-nephritis-quality-measures/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/multi-site-study-evaluating-performance-on-lupus-nephritis-quality-measures/