Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Sacroiliitis is a main radiographic finding in axial spondyloarthritis (axSpA) – the inflammatory rheumatic disease with a strong genetic background. The aim of this study was to evaluate the presence of sacroiliitis in first-degree relatives of patients with ankylosing spondylitis (AS) and to determine fulfilment of Assessment of SpondyloArthritis international Society (ASAS) classification criteria for axial and/or peripheral spondyloarthritis (SpA), and the clinical diagnosis of SpA.
Methods: One hundred subjects without a previous rheumatological diagnosis with a first-degree relative treated for AS were included in the study. Clinical data were collected and rheumatological examinations were performed by trained rheumatologists. Magnetic resonance imaging (MRI) of the sacroiliac joints (SIJ) was read by a trained rheumatologist who was blinded to all patient data. Subjects were further divided into both SpA (according to ASAS classification criteria and clinician opinion) and non-SpA subgroups.
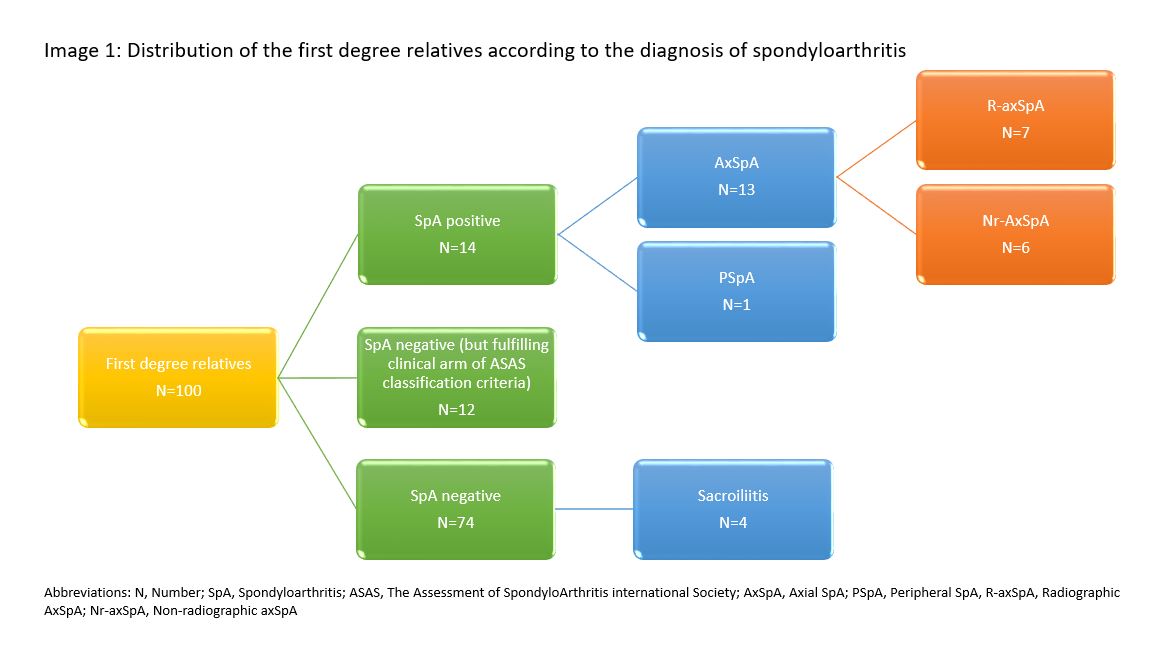
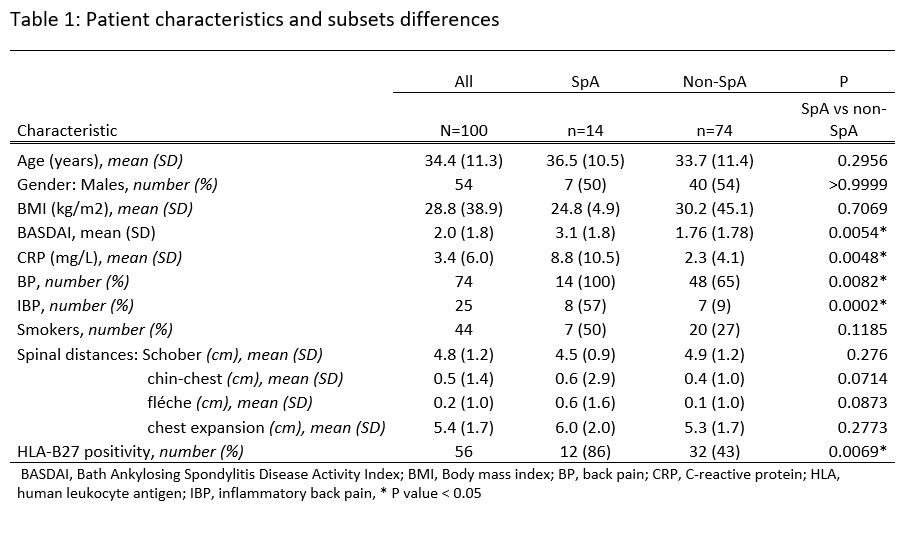
Results: We detected active sacroiliitis defined by MRI in 13 subjects who were further diagnosed with axSpA, 7 (54%) of whom already had advanced radiographic changes on conventional radiographs of the sacroiliac joints. In addition, active sacroiliitis was also present in 4 individuals who did not have back pain. The data are shown in Figure 1. A total of 26 subjects met ASAS classification criteria for SpA, of which the diagnosis of SpA was confirmed in 14 subjects (13 subjects met ASAS classification criteria for axial and 1 subject for peripheral SpA). In addition, 12 individuals met the clinical arm of the ASAS classification criteria for axSpA, but were not diagnosed with axSpA in the clinicians’ opinion. Analysis of clinical characteristics showed a significant difference in CRP and BASDAI between the SpA vs. non-SpA subgroups (8.8 (±10.5) vs. 2.3 (±4.1) mg/l, p=0.0048, and 3.1 (±1.8) vs. 1.76 (±1.78), respectively). Individuals diagnosed with SpA were more likely to be HLA-B27 positive and had inflammatory back pain compared to the non-SpA subgroup (87% vs. 43%, p=0.0069 and 57% vs. 9%, p=0.0002, respectively). Individuals who were not diagnosed with SpA but met the clinical arm of the ASAS classification criteria for axSpA were excluded from the analysis. Other clinical characteristics and differences between subgroups are shown in Table 1.
Conclusion: In this cross-sectional study, 17% of first degree relatives of patients with AS had MRI- defined sacroiliitis, however not all of them were diagnosed with SpA due to the absence of back pain. A quarter of the subjects with first-degree AS relative met the classification criteria for SpA, and 14% were diagnosed with SpA based on physician opinion.
To cite this abstract in AMA style:
Bubova K, Hasikova L, Mintalova K, Gregova M, Forejtova S, Senolt L, Pavelka K. MRI-defined Sacroiliitis in First Degree Relatives of Ankylosing Spondylitis Patients [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/mri-defined-sacroiliitis-in-first-degree-relatives-of-ankylosing-spondylitis-patients/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/mri-defined-sacroiliitis-in-first-degree-relatives-of-ankylosing-spondylitis-patients/