Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Primary systemic vasculitides comprise a group of immunological disorders that inflame blood vessel walls and are categorized by the size of the blood vessels involved (small, medium, and large vessel vasculitis). This group of disorders has an elevated mortality rate among rheumatologic diseases, as prior studies have suggested. While earlier analyses have studied mortality trends related to this group of disorders, newer, more updated research is limited, especially concerning trends beyond 2019.
Methods: Datasets from the CDC WONDER Multiple Cause-of-Death public use records from 1999 to 2023 were used to analyze deaths in adults ≥25 years old, assigning ICD-10 codes (M30 and M31 series) to primary systemic vasculitis by year and place of death, as well as by demographic (sex, age group, race) and regional (state, census region, rural-urban) stratifications. Age-adjusted mortality rates (AAMR) were calculated per 1,000,000 with 95% confidence intervals by standardizing crude mortality rates (CMR). Annual percent change (APC) and average annual percent change (AAPC) were evaluated using Joinpoint regression software.
Results: A total of 39,093 deaths occurred from 1999 to 2023, mostly in medical facilities (61.8%). The AAMR declined from 11.2 in 1999 to 4.9 in 2023 (AAPC: -3.3; 95% CI: -3.6 to -2.9). Women had a higher average AAMR compared to men, along with a higher rate of decrease (AAPC women: -3.4; 95% CI: -3.8 to -3.0; men: -2.9; 95% CI: -3.3 to -2.4). Adults aged ≥65 years had the highest average AAMR, along with the highest rate of decrease among the age groups (AAPC ≥65 years: -3.4; 95% CI: -3.7 to -3.0; 45–65 years: -2.9; 95% CI: -3.5 to -2.4; 25–44 years: -2.2; 95% CI: -3.2 to -1.3).Racially, non-Hispanic (NH) White populations had the highest average AAMR, along with the highest rate of decrease (AAPC NH White: -2.7; 95% CI: -3.3 to -2.2; NH Asian/Pacific Islander: -2.9; 95% CI: -3.8 to -2.0; Hispanic/Latino: -3.0; 95% CI: -3.7 to -2.1; NH Black/African American: -3.3; 95% CI: -4.0 to -2.6).Regionally, the Midwest had the highest average AAMR, though the South had the highest rate of decrease (AAPC South: -3.4; 95% CI: -3.8 to -3.0; West: -2.8; 95% CI: -3.6 to -2.1; Midwest: -3.1; 95% CI: -3.6 to -2.6; Northeast: -3.2; 95% CI: -3.7 to -2.7).From 1999 to 2020, state-wise AAMRs ranged from 5.1 in Hawaii to 12.6 in Vermont. From 2021 to 2023, AAMRs ranged from 3.7 in Louisiana to 11.8 in Minnesota. From 1999 to 2020, rural areas had a higher average AAMR, though urban areas had a higher rate of decrease (AAPC urban: -3.8; 95% CI: -4.1 to -3.4; rural: -2.5; 95% CI: -3.0 to -2.0).
Conclusion: Though primary systemic vasculitis-related mortality rates in adults declined from 1999 to 2023, disparities across demographic and regional groups remain, highlighting the need for targeted prevention and support systems to improve outcomes in at-risk communities.
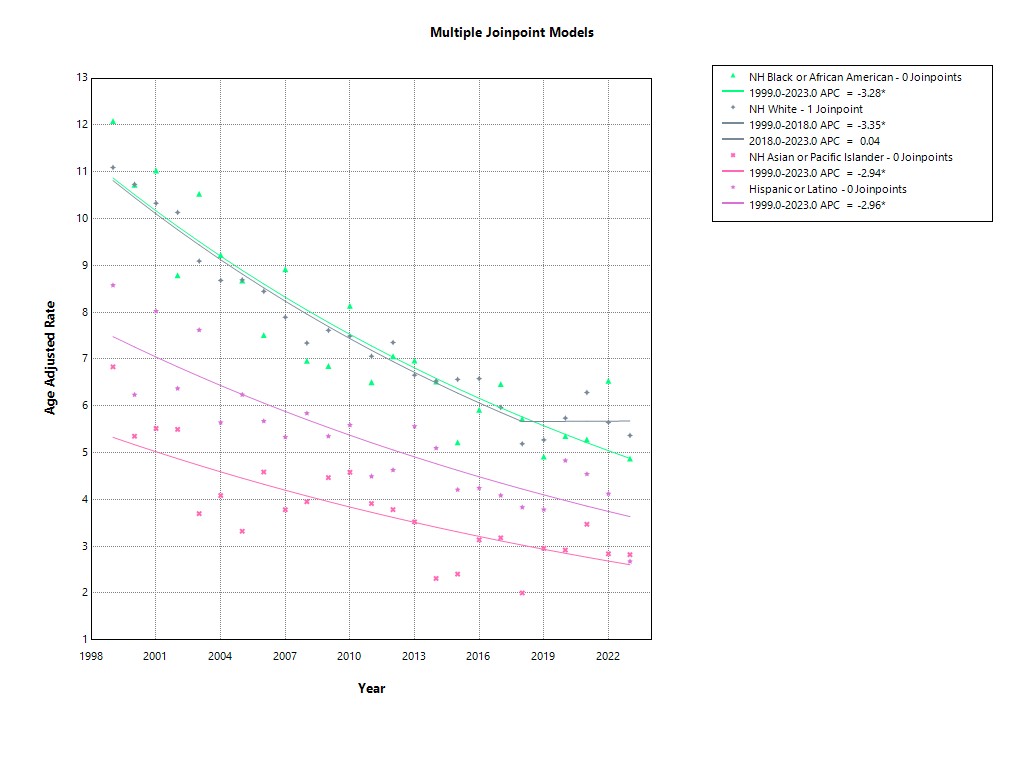 Trends in Vasculitis-Related Mortality by Race, United States (1999–2023)
Trends in Vasculitis-Related Mortality by Race, United States (1999–2023)
.jpg) Primary Systemic Vasculitis Mortality by Sex (1999–2023)
Primary Systemic Vasculitis Mortality by Sex (1999–2023)
.jpg) Primary Systemic Vasculitis Mortality by Census Region (1999–2023)
Primary Systemic Vasculitis Mortality by Census Region (1999–2023)
To cite this abstract in AMA style:
Qasim R, Mohib S, Ali M, Mohib K. Mortality Trends in Primary Systemic Vasculitis in the United States (1999–2023) [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/mortality-trends-in-primary-systemic-vasculitis-in-the-united-states-1999-2023/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/mortality-trends-in-primary-systemic-vasculitis-in-the-united-states-1999-2023/
