Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Autoimmune interstitial lung disease (ILD) may arise in various autoimmune rheumatic diseases (ARD). Some patients develop ILD with systemic symptoms and autoantibodies without fulfilling ARD criteria, as in interstitial pneumonia with autoimmune features (IPAF) and unclassifiable autoimmune ILD (ILD-UA). Autoinmune-ILD can progress to progressive pulmonary fibrosis (PPF), characterized by irreversible lung damage and high mortality. Real-world data on these patients, particularly cause-specific mortality, are still limited. This study evaluates ILD-related mortality rate over time in patients with autoimmune ILD from the onset of PPF.
Methods: A multicenter longitudinal study was conducted on patients with autoimmune origin ILD (ARD-ILD, IPAF, and ILD-UA), from Madrid, enrolled from Jun 2006 to Jun 2023 and followed up until Sept 2024. Autoimmune-ILD patients were included in a registry [pNEumology RhEumatology Autoinmune diseases (NEREA)]. Patients were required to meet progressive pulmonary fibrosis (PPF) criteria based on the ATS/ERS/JRS/ALAT Guideline. Main outcome was specific-cause mortality related to ILD. Covariables included sociodemographic, clinical, radiological, pulmonary function tests, and therapy. Time of observation comprised the period from the PPF starting until loss of follow-up, main outcome or end of study. Survival techniques were used to estimate the specific-cause mortality rate related to ILD (MR), expressed per 100 patients-year with their respective 95% confidence interval [CI].
Results: A total of 158 patients with PPF were included, of whom 62% were women (n=98). Autoimmune diseases were present in 71.5%, with rheumatoid arthritis being the most common (39.9%) followed by systemic sclerosis (12.0%). Regarding treatments at baseline, 70.9% received corticosteroids, 70.3% disease-modifying antirheumatic drugs (DMARDs) (csDMARDs: 54.4%, b/tsDMARDs: 31.7%), and 14.6% antifibrotic therapy. During follow-up, a total of 47 deaths were recorded. Of these, 37 (78.7%) were attributed to ILD-related causes, with respiratory failure being the most common (16.2%). Additional causes included cancer (n=4), sepsis(n=2), cardiovascular(n=1), neurological(n=2), and unknown(n=1). The ILD-specific mortality rate was 6.2 [4.5-8.5], with a median survival time of 7.8 years. The MR was similar between genders and higher at older ages. Regarding radiographic patterns it was higher in UIP (9.9 [7.0-14.2]) compared to NSIP (MR: 0.47 [0.06-3.4]); in diagnosis MR was higher in IPAF/UA (MR: 7.7 [4.2-13.9]), RA (MR: 9.2 [6.0-14.2]) and lower in others (scleroderma MR:1.5 [0.4-6.3]). Concerning therapy, MR was lower in those on DMARDs during the follow-up compared to those with none (MR: with 4 [2.5-6.4]; without 9.0 [5.7-14.3]).
Conclusion: This study provides real-world evidence on the clinical course and cause-specific mortality in patients with autoimmune PPF-ILD. The findings underscore the substantial mortality rate directly attributable to ILD. Moreover, the results suggest a potential survival advantage in patients receiving immunomodulatory therapy, supporting its role in the management of this patient population.
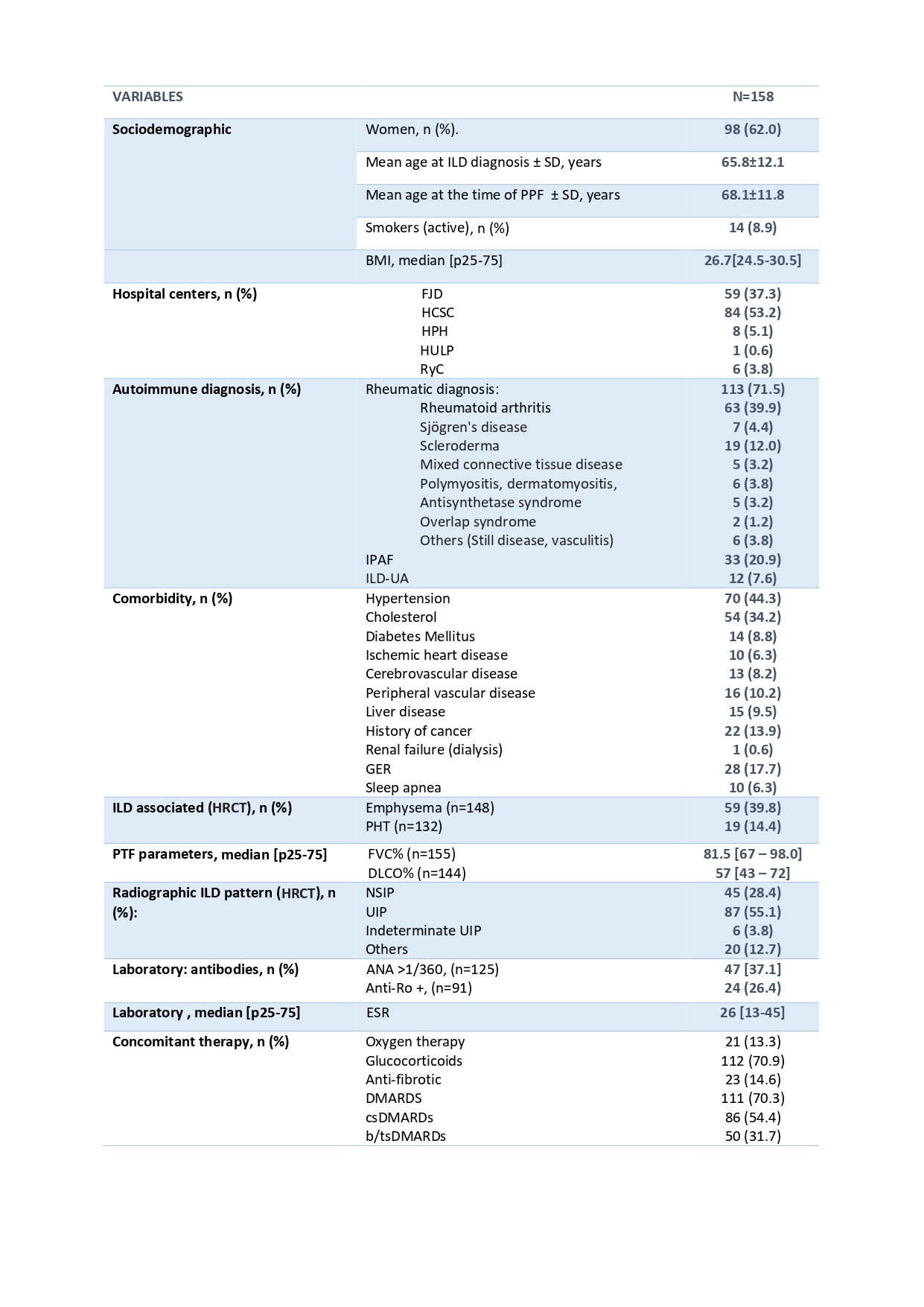 Table 1: Baseline sociodemographic, clinical, functional, radiologic characteristics of the patients.
Table 1: Baseline sociodemographic, clinical, functional, radiologic characteristics of the patients.
To cite this abstract in AMA style:
Ruiz-Valdepeñas Almansa M, DE MIGUEL C, FREITES D, Vadillo Font C, Nieto M, Sanchez Pernaute O, Romero-Bueno f, Rodriguez-Nieto M, Laporta R, Godoy Tundidor H, Loarce J, A Rigual J, Abasolo Alcazar l. Mortality In Progressive Pulmonary Fibrosis Associated to Autoimmune Diseases: NEREA Registry [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/mortality-in-progressive-pulmonary-fibrosis-associated-to-autoimmune-diseases-nerea-registry/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/mortality-in-progressive-pulmonary-fibrosis-associated-to-autoimmune-diseases-nerea-registry/
