Session Information
Date: Saturday, November 16, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Idiopathic Inflammatory Myopathies (IIMs) are a group of heterogeneous connective tissue diseases including dermatomyositis (DM), polymyositis (PM), anti-synthetase syndromes (ASS), immune-mediated necrotizing myopathies (NM), and overlap syndromes (OS). These diseases are the most severe connective tissue diseases, with a high mortality rate of 30%. Mortality risk between these different subgroups is not well-known.
The purpose of this study was to evaluate the mortality rate and cumulative incidence of mortality in IIM and its subgroups.
Methods: A retrospective study was conducted using the MIIRTALITY cohort, including patients followed for IIM from 2010 to 2022. Patients were included if they had more than one year of follow-up or early death, were diagnosed between 2010 and 2020, and met the 2017 EULAR and/or 2019 ENMC classification criteria. They were then categorized into five subgroups: DM, PM, ASS, NM, and OS.
We compared IMM-patients characteristics’ within each subgroups. Survival analysis based on IMM subgroups was performed using the Kaplan-Meier method. Univariable and multivariable Cox proportional hazards models (ascending step-by-step method) were used to determine baseline variables associated with mortality.
Results: 225 patients were included, divided into 83 DM (36.9%), 14 PM (6.2%), 55 ASS (24.4%), 24 NM (10.7%), and 49 OS (21.8%). The median age was 59 years [46–69 years], with a female predominance (n = 133, 59.1%). The median follow-up duration was 4 years [2–7 years]. Cancer was associated with 29 patients (12.8%).
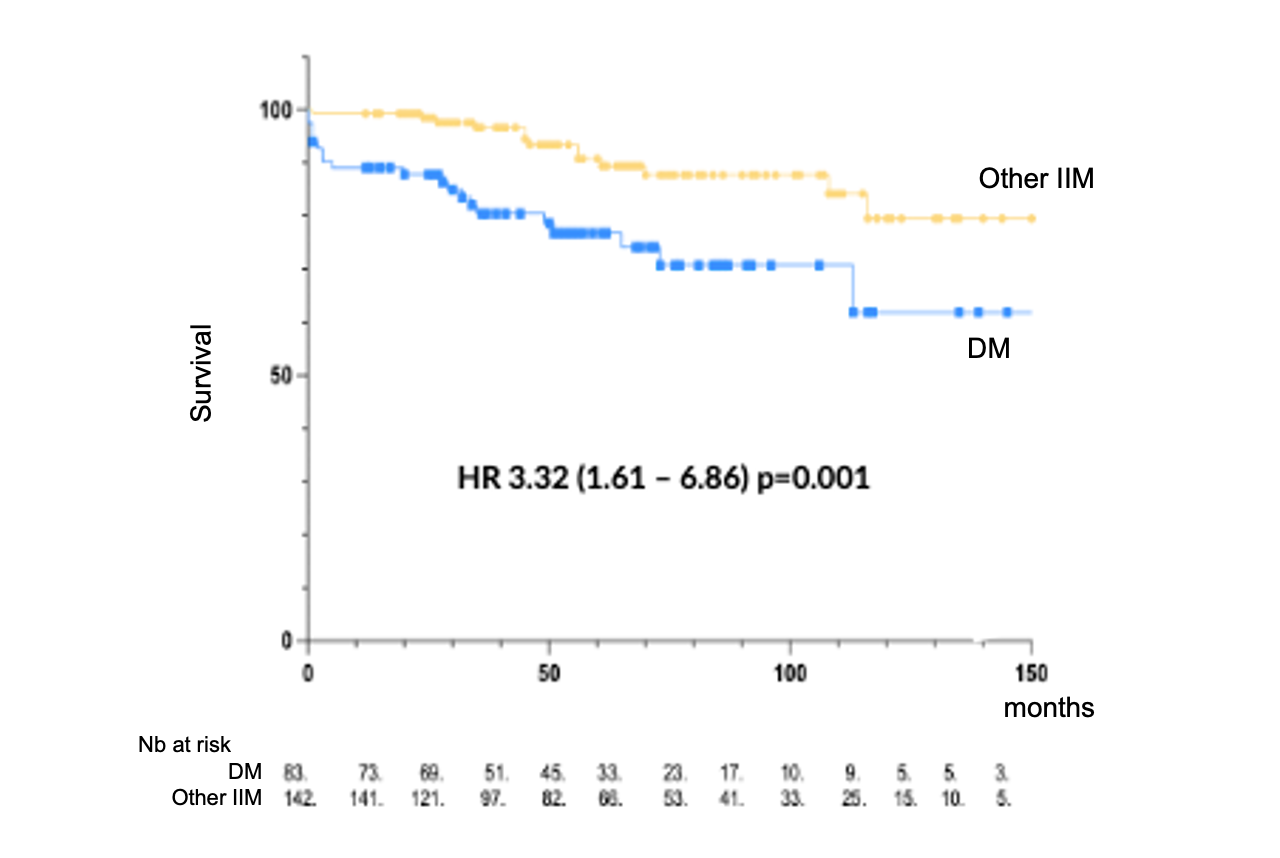
The mortality rate of IIM in our cohort was 14.7%, with a cumulative incidence of 3.1 per 100 person-years. The overall survival probability was 95.5% at 1 year, 85.5% at 5 years, and 73% at 10 years. Comparative analysis showed a significant difference between subgroups (p = 0.03), with higher mortality in the dermatomyositis group compared to other subgroups, with a significant difference and an HR of 3.32 (95% CI 1.61–6.86) (figure 1). Anti-synthetase syndromes had the best prognosis with an HR of 0.41 (95% CI 0.19–0.88). There was no difference in mortality among the other subgroups. Causes of death included infections (30.3%, 10 patients), cancer and pulmonary causes (18.2%, 7 patients), and cardiac causes (9%, 3 patients). Risk factors for mortality in IIM included cancer association with an HR of 12.2 (95% CI 3.09–48.13). A protective factor was having an IIM other than dermatomyositis (HR 0.37, 95% CI 0.18–0.76).
Conclusion: The 14.7% mortality rate found in our study is one of the lowest among IIM cohort studies, likely due to the recent nature of our study and improved management in recent years. Comparison between subgroups shows that dermatomyositis is the IIM subgroup with the highest mortality rate. Anti-synthetase syndromes have the best prognosis. Improving knowledge of these diseases is important for better characterizing the different subgroups with distinct phenotypes and prognoses. This underscores the importance of personalized care tailored to each patient, with increased surveillance, especially for dermatomyositis, and continued therapeutic management improvements to enhance survival in these patients.
To cite this abstract in AMA style:
Larrauffie A, Bost C, Faruch M, Uro-coste E, Prevot G, Villeneuve T, Zordan J, Barrier C, Mourguet M, Guille M, Sailler L, Alric L, De Almeida Chaves S, Pugnet G. Mortality: Comparison, Causes and Determinants in Subgroups of Idiopathic Inflammatory Myopathies [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/mortality-comparison-causes-and-determinants-in-subgroups-of-idiopathic-inflammatory-myopathies/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/mortality-comparison-causes-and-determinants-in-subgroups-of-idiopathic-inflammatory-myopathies/