Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Ethnicity and health outcomes are intrinsically interrelated, although mechanisms are complex. Systemic lupus erythematosus (SLE) is a disease with higher incidence in non-White populations and associated with premature mortality. Survival is thought to vary across ethnicities in patients with SLE; however, there has not been a comprehensive review or meta-analysis demonstrating this. Thus, we aimed to investigate the association between ethnicity and mortality in patients with SLE.
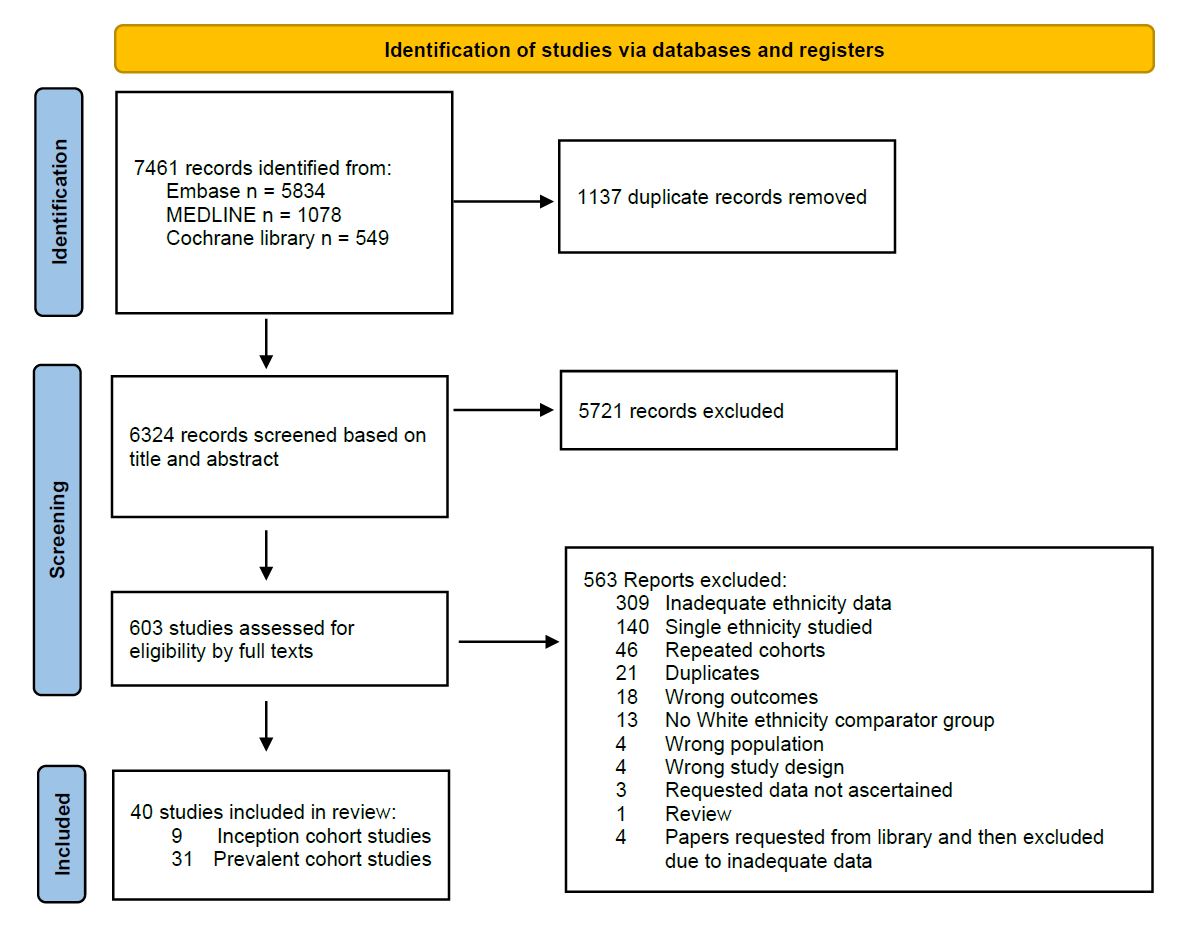
Methods: We performed a systematic literature search of the databases MEDLINE, Embase and the Cochrane Library, from inception to 31 December 2023. Search terms included systemic lupus erythematosus, ethnicity, race, mortality and synonyms. Study eligibility criteria were cohort studies and trials that reported on the mortality of adults >16 years old with SLE. We used a pairwise meta-analysis to determine the pooled odds ratio of death for those from Black, Asian, Hispanic or Indigenous ethnic groups compared to those of White ethnicity, recognising that non-White ethnicities represented underserved populations.
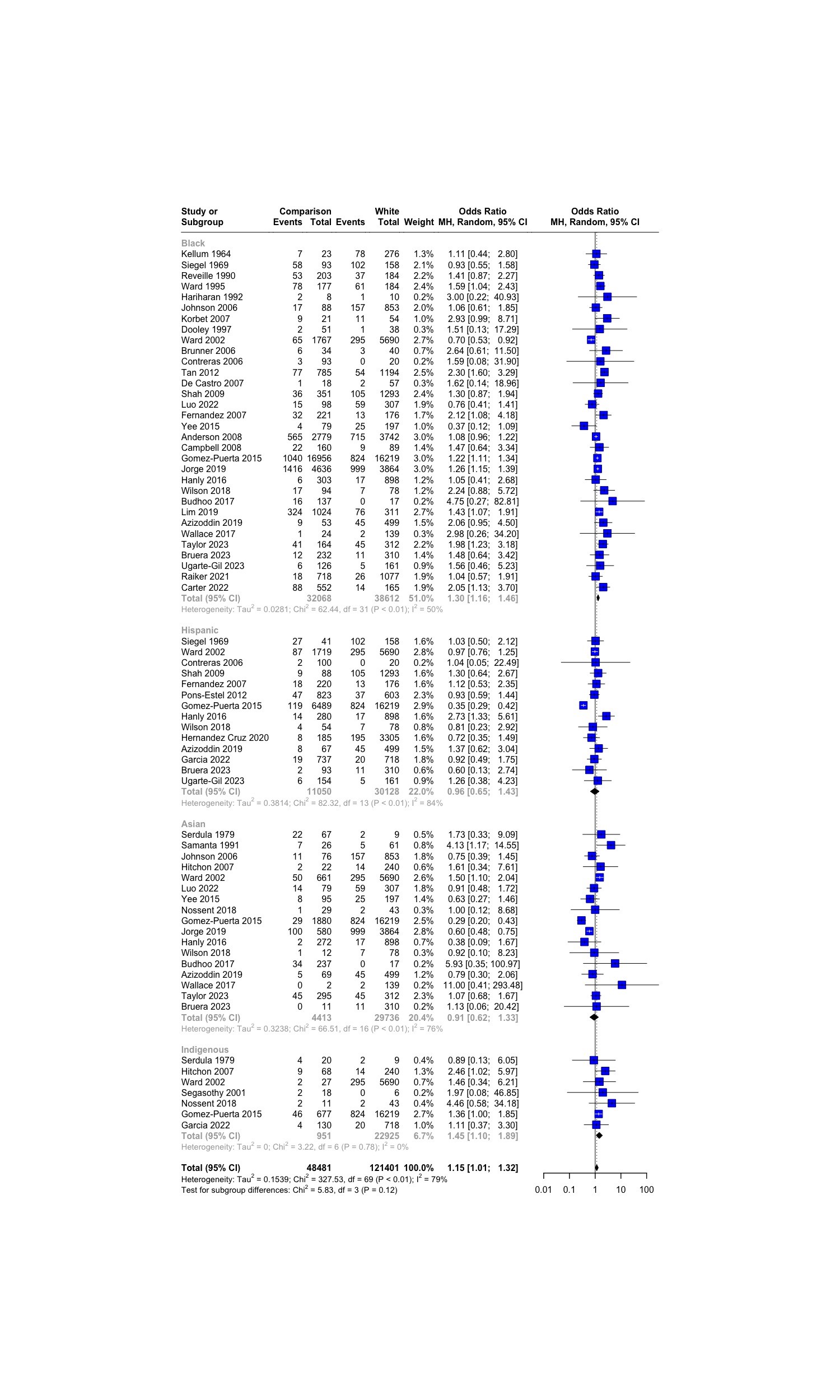
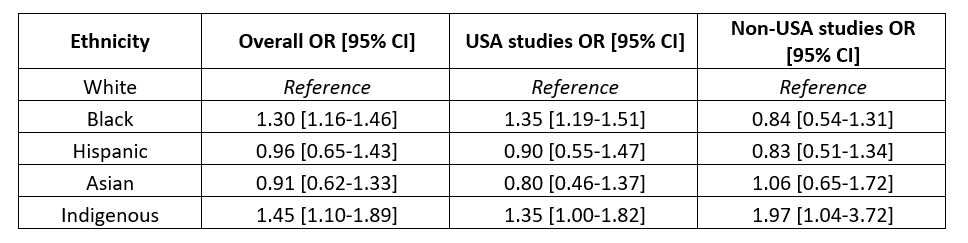
Results: Forty studies, comprising 92,079 patients with SLE were included (Figure 1). Overall, non-White ethnicity was significantly associated with death compared to White ethnicity (OR 1.15 [95% CI: 1.01-1.32]; Figure 2). On subgroup analysis, mortality was higher in Black patients (OR 1.30 [95% CI: 1.16-1.46]) and Indigenous patients (OR 1.45 [95% CI: 1.10-1.89]), whilst Asian and Hispanic patients showed no significant differences compared to White patients with SLE (Table 1). Meta-regression found no associations between study effect size, length of follow-up or mid-year point. The association between ethnicity and mortality in patients with SLE did not appear to change over time. Sixty-five percent of included studies were conducted in the United States of America (USA) and when excluded, the significant difference in mortality between Black and White individuals with SLE was no longer seen (OR 0.84 [95% CI: 0.54-1.31]; Table 1).
Conclusion: Patients with SLE from Black or Indigenous ethnicities had higher mortality than those from White ethnicities. This could be driven by several complex and diverse factors such as structural racism, associated socioeconomic deprivation, healthcare accessibility, differing cultural beliefs or more severe SLE phenotypes in these ethnic groups. However, on sensitivity analyses we observed inconsistencies between USA and non-USA cohorts regarding the association of Black ethnicity and mortality, though a scarcity of data outside of the USA was noted. Recent national data from the USA described higher mortality in the general Black and Indigenous American population compared to the White American population, suggesting a wider systemic issue which may be reflected in, but not limited to, patients with SLE. Until more generalisable data outside of the USA are available, we promote caution in the use of ethnicity as a risk factor for mortality.
To cite this abstract in AMA style:
Patel S, Yang Z, Nagra d, Adas M, Russell M, Norton S, Wincup C, Galloway J, Bramham K, Gordon P. Mortality and Ethnicity in Adults with Systemic Lupus Erythematosus: A Systematic Literature Review and Meta-Analysis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/mortality-and-ethnicity-in-adults-with-systemic-lupus-erythematosus-a-systematic-literature-review-and-meta-analysis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/mortality-and-ethnicity-in-adults-with-systemic-lupus-erythematosus-a-systematic-literature-review-and-meta-analysis/