Session Information
Date: Sunday, November 10, 2019
Title: 3S108: RA – Diagnosis, Manifestations, & Outcomes II: Cardiovascular Comorbidities (921–926)
Session Type: ACR Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Rheumatoid arthritis (RA) patients are at increased risk of cardiovascular disease (CVD). Methotrexate (MTX), a mainstay in the treatment of RA, appears to mitigate this risk. However, prior studies have been limited in their ability to account for the effects of disease activity and examine the mechanisms that account for CVD risk reduction. We aimed to determine whether the association of MTX with reduced CVD risk was related to modulation of disease activity or direct effects.
Methods: We observed participants in a prospective, multicenter cohort of US Veterans with RA for incident CVD events from 4/2005 to 4/2015. CVD events were defined as a composite of acute myocardial infarction (AMI), coronary revascularization, stroke, and hospitalization for heart failure (CHF). These were identified using diagnostic and procedure codes from inpatient and outpatient encounters (validated by medical record review) and the National Death Index. Demographics, traditional CVD risk factors, comorbidities (including hypertension, hyperlipidemia, diabetes, chronic kidney disease, liver disease, and prior CVD), as well as aspirin, statin, and NSAID use were assessed using registry and administrative data. MTX (and other DMARD/prednisone) exposure was defined at each visit by linking to pharmacy dispensing data, including a 90-day grace period upon discontinuation. To reduce confounding by disease activity, we used marginal structural models incorporating disease activity from the prior visit into the propensity to receive MTX to determine the overall association of MTX with CVD events. To examine whether the association of MTX use with CVD was mediated through disease activity, we used sequential Cox models including post-MTX disease activity.
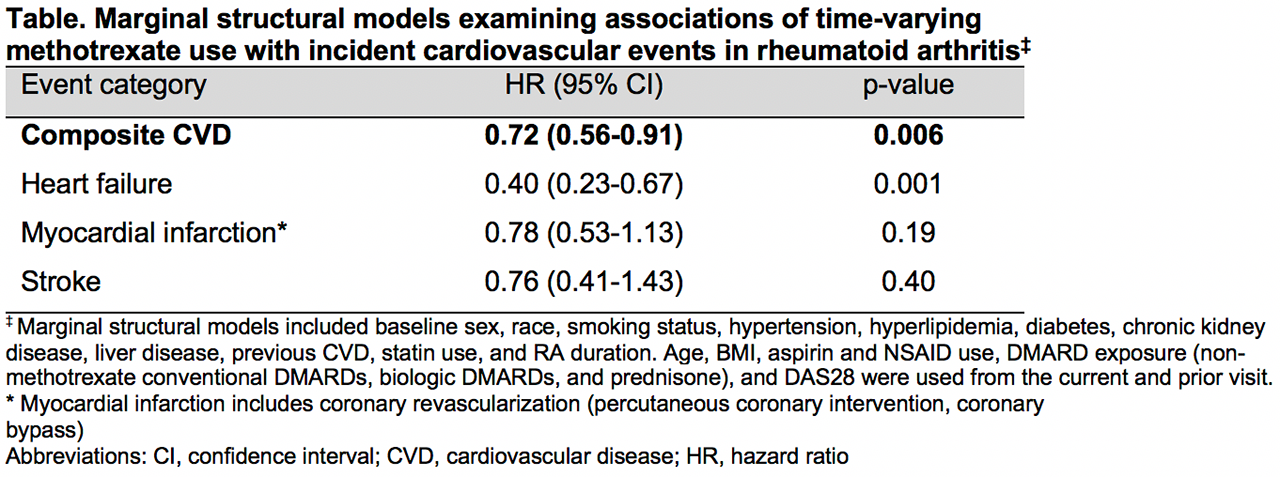
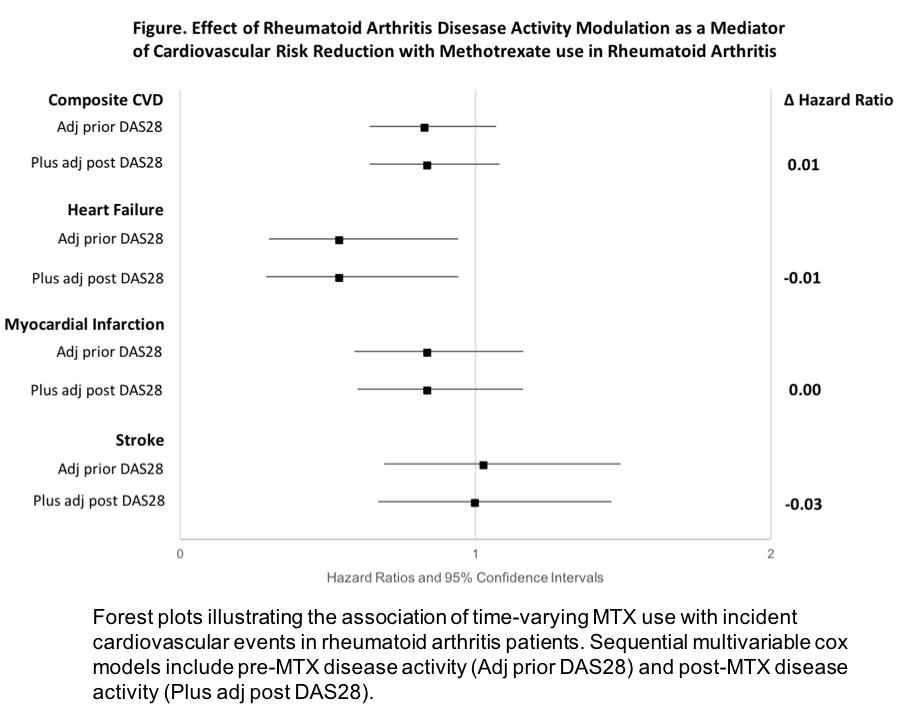
Results: RA patients (n=2168) were predominantly older (mean age 64 years), male (90%), frequent smokers (80% current/former), seropositive (79% RF, 78% anti-CCP), with moderate baseline disease activity (mean DAS28 3.7). The incidence of composite CVD events (n=401) was lower in MTX exposed patients (33.8/1000 person-years) vs. MTX non-exposed patients (40.7/1000 person-years). Using marginal structural models to account for disease activity at the prior visit, MTX use was associated with reduced risk of composite CVD events (HR 0.72, 95% CI 0.55-0.89) and CHF (HR 0.40, 95% CI 0.23-0.67), with a trend toward reduced risk of AMI and stroke (Table). In sequential multivariable Cox models to assess direct and indirect effects, adjustment for post-MTX disease activity did not significantly alter the association of MTX use with composite or individual CVD events (range ΔHR -0.03 to 0.01, Figure).
Conclusion: In a multicenter RA cohort, MTX use was associated with a 30% reduced risk of composite CVD events and a 60% reduced risk of CHF hospitalizations. The protective effect of MTX was independent of other factors including treatment-related changes in disease activity, suggesting that additional mechanisms mediate CVD risk reduction with MTX in RA. This should be considered when selecting DMARD therapy regimens in RA patients.
To cite this abstract in AMA style:
Johnson T, Baker J, Roul P, Sayles H, Cannon G, Sauer B, Mikuls T, England B. Methotrexate Is Associated with Reduced Cardiovascular Risk in Rheumatoid Arthritis Independent of Disease Activity Modification [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/methotrexate-is-associated-with-reduced-cardiovascular-risk-in-rheumatoid-arthritis-independent-of-disease-activity-modification/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/methotrexate-is-associated-with-reduced-cardiovascular-risk-in-rheumatoid-arthritis-independent-of-disease-activity-modification/