Session Information
Title: Systemic Lupus Erythematosus - Clinical Aspects and Treatment: Cardiovascular Disease and Pregnancy
Session Type: Abstract Submissions (ACR)
Background/Purpose:
A high prevalence of metabolic syndrome (MetS) has been observed in Systemic Lupus Erythematosus (SLE) patients, but there are scarce data about the main factors for MetS in young patients. The aim of the present study was to evaluate MetS frequency in premenopausal SLE patients and to identify factors that could contribute to this condition.
Methods:
One hundred and three female SLE patients (fulfilled the revised American College of Rheumatology criteria) with age less than 40 years old were selected. Demographical, clinical, laboratorial and therapeutics data about SLE and MetS were assessed. Thirty-five healthy female age-matched were selected as controls. MetS was defined according to the 2009 Joint Interim Statement. Data analysis (SAS 9.3): t Student’s test or Mann-Whitney’s test (continuous data) and chi-square test or Fisher’s exact test (categorical variable) was performed as appropriate. Multivariate analysis used the Poisson regression.
Results:
A higher frequency of MetS (22.3 vs. 5.7%, p=0.03) was observed in SLE group even as higher mean homeostasis model assessment index (HOMA-IR) (1.8 ± 0.9 vs. 1.3 ± 1.0, p=0.0008) and mean systematic coronary risk evaluation (SCORE) risk (1.4 ± 0.8 vs. 1.1 ± 0.4, p=0.01). Regarding MetS criteria, hypertension (42.7 vs 2.9%, p<0.0001) and waist circumference (83.5 vs 37.1%, p<0.0001) were most frequently observed in SLE group. The comparison of SLE patients with and without MetS showed no differences in mean disease duration and damage index score but higher SLE Disease Activity Index (SLEDAI) scores (median [range] 2 [0-31] vs. 2 [0-14], p=0.006) and more frequently previous (73.9 vs. 51.2%, p=0.05) and current renal (34.8 vs. 10.0%, p=0.008) disease in MetS-SLE group. MetS-SLE patients had higher current prednisone dose (20 [0-60] vs. 5 [0-60] mg/dl, p=0.018), cumulative dose (41.48 ± 27.81 vs. 24.7 ± 18.66 g, p=0.023) but no differences in the duration of its use or methylprednisolone pulse use. A higher frequency of chloroquine use was identified in SLE patients without MetS (90.0 vs. 65.2%, p=0.008). In multivariate analysis, only current chloroquine use (prevalence ratio [PR]=0.29; 95% confidence interval [CI] 0.13–0.64) and cumulative prednisone dose (PR=1.02; 95% CI 1.01–1.04) were associated with MetS in SLE. Patients that were not using chloroquine had a 3.48-fold higher risk of MetS and the prevalence of MetS increased by 2% for each increase of one gram of cumulative prednisone dose. The chloroquine use reduced the estimated prevalence of MetS even in patients on steroids and this benefit appears to be greater the higher the cumulative dose of prednisone (figure below): 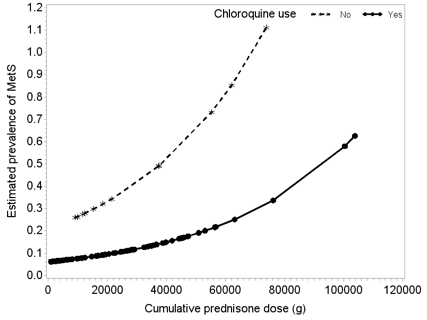
Conclusion:
The prevalence of MetS is high in premenopausal SLE patients and is mainly influenced by lupus therapy with prednisone or chloroquine rather than disease itself. Chloroquine use appears to decrease MetS prevalence even in patients on steroids.
Disclosure:
L. Muniz,
None;
R. M. R. Pereira,
None;
T. Silva,
None;
E. Bonfá,
None;
E. F. Borba,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/metabolic-syndrome-in-young-premenopausal-female-lupus-patients-is-mainly-influenced-by-therapies/
