Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
all-cause and cardiovascular mortality and cardiovascular morbidity are reportedly increased in rheumatic diseases, both inflammatory and non-inflammatory. Few studies, however have addressed the impact of metabolic syndrome (MetS) on mortality and cardiovascular morbidity (ASCVD, death, stroke, Myocardial infarction, peripheral arterial disease) in rheumatic diseases.Methods:
MetS was defined according the 2009 Consensus criteria (1), as the presence of at least among 3 among increased abdominal circumference (AC: M ≥ 94 cm; F ≥ 80 cm) , elevated blood pressure (BP: ≥130/85), triglycerides (TG ≥150 mg/dL), glucose (GLU: ≥100 mg/dL), or reduced HDL-Cholesterol (HDL M<40 F<50 mg/dL). The original population consisted of 1234 non-selected rheumatic patients without a history of major cardiovascular. 259 patients were eventually excluded from data analysis, because of lack of follow-up (N=252) or evidence of cardiovascular events before inclusion in the study (N=7). Of the remaining 975 patients (M 217; F 758), complete data were available for 849 patients; Mets variables were missing in < 5% of patient (AC 2.15%; BP 2.36%; GLU 3.79%; HDL 4.52%; TG 3.90%). According to current practice (2), missing data were imputed by multiple imputation, using the multivariate imputation by chained equation algorithm (3). Survival and ASCVD event risk were evaluated by Kaplan-Meier and Cox proportional hazard models. Statistical computations were performed with SPSS and R softwares.Results:
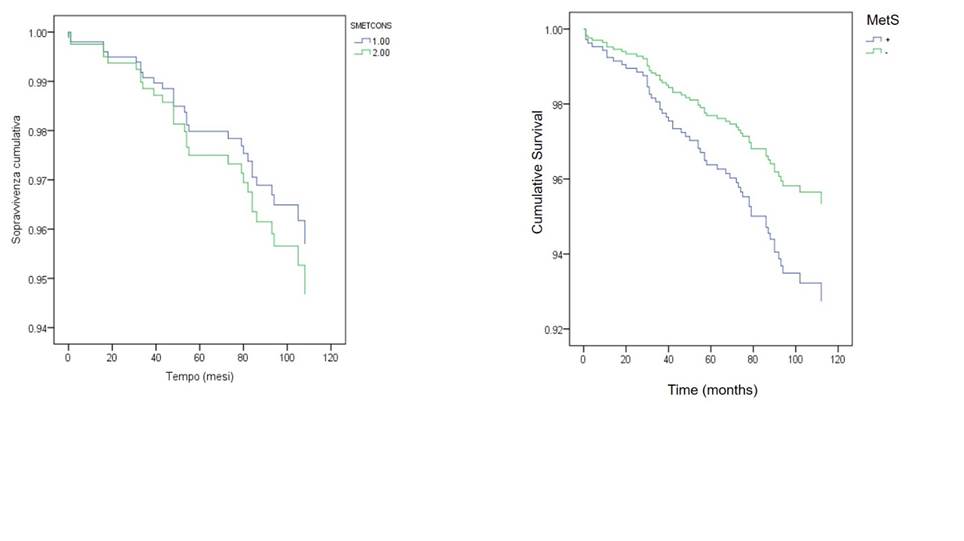
The mean duration of follow-up was 7.38 years (0-1 – 11.67), totalling 7195 patient-year. 219 (22.5%) were affected by non inflammatory diseases, 260 (26.7%) by RA, 152 (15.6%) by psoriatic arthritis/SpA, and 344 (35.3%) by CTD or vasculitis. In the whole population, 63 deaths and 115 ASCVD events in 58 patients were observed, with no significant differences between MetS + (N=330) and MetS- (N=645) patients. In the Cox Model, Mets was not correlated with the risk of death (HR 0.996 95% CI 0.577-1.721, p = 0.989), or ASCVD (HR 1.514, 95% CI 0.876-2.617, p = 0.138). For both all-cause mortality and ASCVD, age (HR 1.103, 95% CI 1.073-1.134, and HR 1.983 95% CI 1.095-3.591 respectively) and male sex (HR 1.943, 95% CI 1.066-3.541 and HR 1.046 95% CI 1.021-1.072 respectively) were correlated with the outcome.
Conclusion: In our population patients affected by non-selected rheumatic diseases, metabolic syndrome did not influence all-cause deaths and atherosclerotic cardiovascular events. These data seem to confirm previous observations showing that factors other than traditional risk factors have a major impact on cardiovascular mortality and morbidity in rheumatic diseases. References
(1) Alberti, K.G., et al., Circulation, 2009. 120: 1640-1645.
(2) van der Heijden, G. J., et.al. J Clin Epidemiol 2006. 59: 1102-9.
(3) van Buuren, S. Stat Methods Med Res , 2007. 16: 219-242.
To cite this abstract in AMA style:
Antivalle M, Varisco V, Mutti A, Batticciotto A, Ditto MC, Atzeni F, Sarzi-Puttini P. Metabolic Syndrome, All Cause Mortality and Atherosclerotic Cardiovascular Disease in Rheumatic Diseases [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/metabolic-syndrome-all-cause-mortality-and-atherosclerotic-cardiovascular-disease-in-rheumatic-diseases/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/metabolic-syndrome-all-cause-mortality-and-atherosclerotic-cardiovascular-disease-in-rheumatic-diseases/