Session Information
Date: Friday, November 6, 2020
Title: Spondyloarthritis Including Psoriatic Arthritis – Treatment Poster I
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Recreational legalization of cannabis has influenced the medical use by patients. When only legal medical access was available in Canada, 4.3% of all rheumatology patients reported medical use, with this number increasing to 12.6% following recreational legalization. In this study we examine the prevalence of medical cannabis use and explore factors associated with medical use in patients with ankylosing spondylitis (AS).
Methods: During a two-month period (April-May 2019), consecutive patients attending an academic, community-based rheumatology clinic staffed by 3 rheumatologists participated in an onsite survey comprising 2 questionnaires: 1) demographic and disease information completed by the rheumatologist, 2) patient anonymous questionnaire of health status, cannabis use (recreational and/or medicinal) and characteristics of use.
Results: In a cohort of 1000 rheumatology attendees (73% females; mean age 64 ± 14 yrs), medical cannabis (MC) had ever been used by 12.6% (95% CI: 10.7%-14.8%) with half continuing use. Inflammatory arthritis was diagnosed in 621 (62%), with 72 (7.2%) diagnosed with AS. Characteristics of AS patients are shown in Table 1. Of the 72 AS patients, 17 (24%) had used MC (95% CI: 14.4-35.1), with 9 (53%) continuing medical use. Past and current recreational cannabis use for all AS patients was 31 (43.1%) and 8 (11.1%) respectively, with no difference in ever recreational rates for medical users. AS users vs. AS non users did not differ for demographic or employment data; there was a trend for users to have more concomitant FM 35.3% vs 12.7% (p=0.065), used significantly more medication types 2.4 vs. 1.2 (p< 0.001), used more opioids 23.5% vs. 5.5% (p=0.049), had a poorer patient global assessment 5.3 vs. 3.6 (p=0.022) and had more pain 6.5 vs 4.4 (p=0.015). Inhalation was the most common method of medical cannabis use. Symptom relief was 5.1±2.1 on a 10 cm VAS.
Conclusion: AS patients had double the rate of medical cannabis use compared to other rheumatology patients. Poorly controlled pain may be the driver for an increased MC in AS, although the effect was perceived as modest.
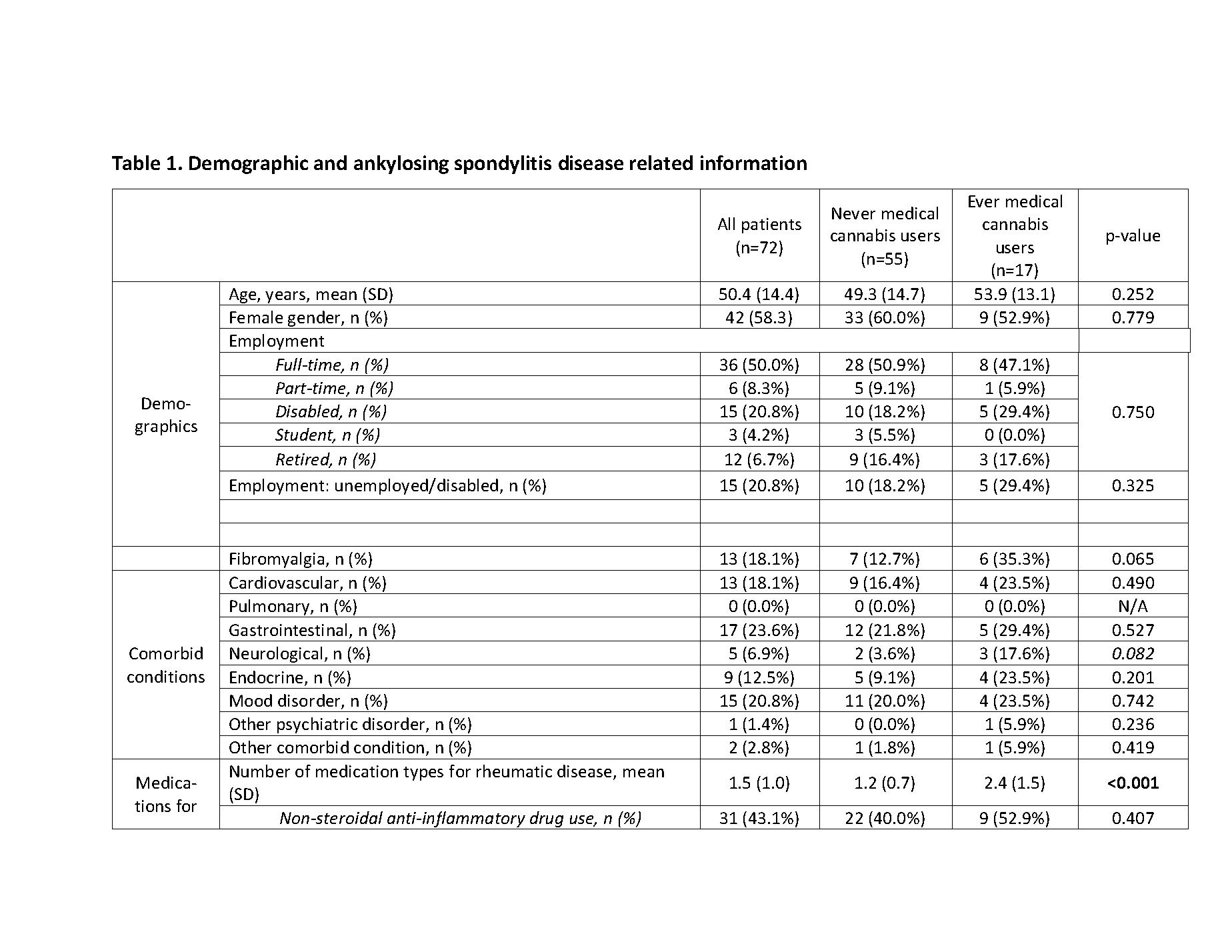 Table 1. Demographic and ankylosing spondylitis disease related information (part 1)
Table 1. Demographic and ankylosing spondylitis disease related information (part 1)
 Table 1. Demographic and ankylosing spondylitis disease related information (part 2)
Table 1. Demographic and ankylosing spondylitis disease related information (part 2)
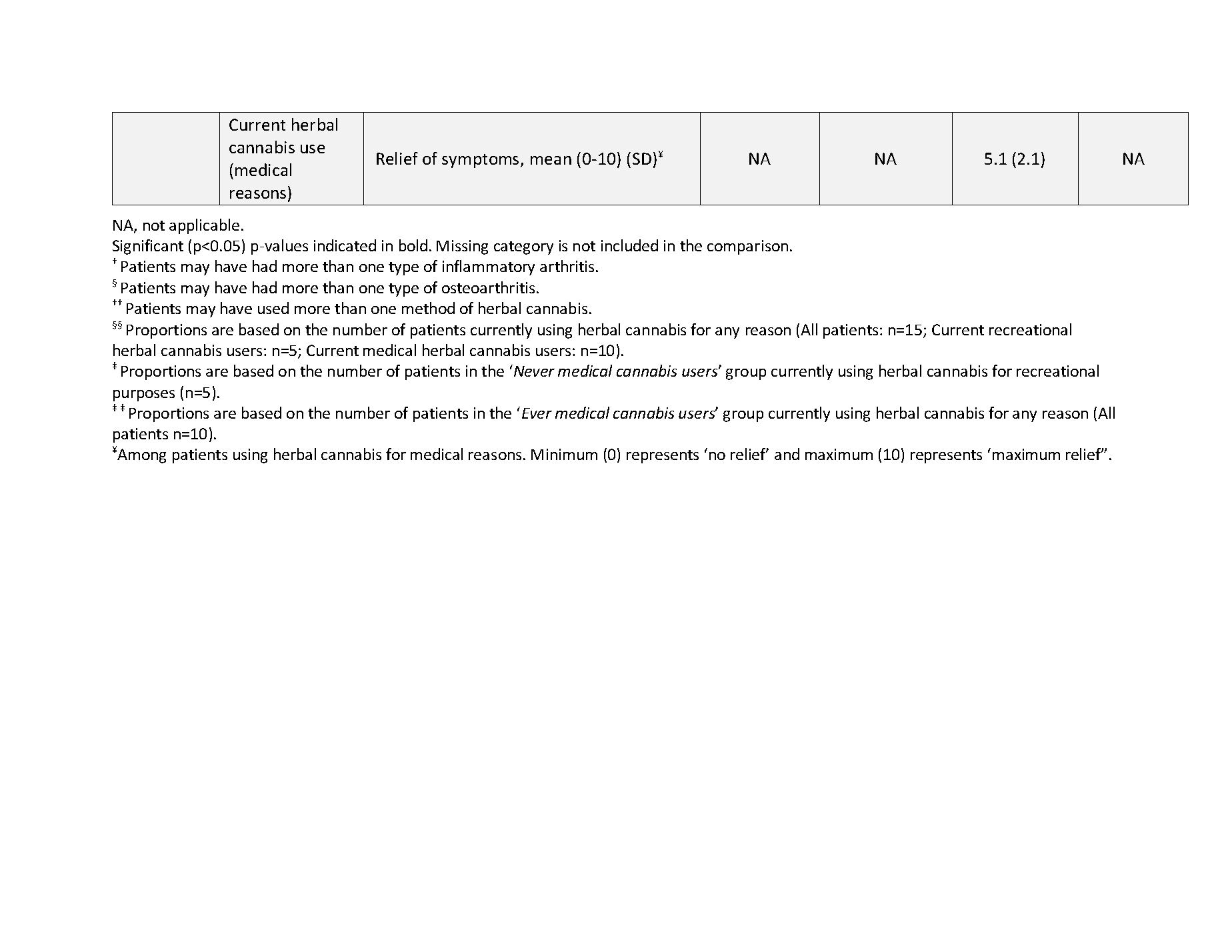 Table 1. Demographic and ankylosing spondylitis disease related information (part 3)
Table 1. Demographic and ankylosing spondylitis disease related information (part 3)
To cite this abstract in AMA style:
Rampakakis E, Shir Y, Sampalis J, Cohen M, Starr M, Häuser W, Fitzcharles M. Medical Cannabis in Ankylosing Spondylitis Following Recreational Legalization: A Prospective Cross-sectional Study [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/medical-cannabis-in-ankylosing-spondylitis-following-recreational-legalization-a-prospective-cross-sectional-study/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/medical-cannabis-in-ankylosing-spondylitis-following-recreational-legalization-a-prospective-cross-sectional-study/
