Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Data on birth outcomes to women with rheumatoid arthritis (RA) are limited and conflicting. Some studies indicate that women with well controlled RA have birth outcomes similar to the general population, while others show higher rates of preterm birth and cesarean section. There are few studies assessing how RA impacts maternal peripartum outcomes such as maternal infection rates and blood transfusions. Using a real-world, electronic health record (EHR) cohort, we assessed RA medication use, fetal, and maternal peripartum outcomes.
Methods: In a large, de-identified EHR with over 3 million subjects and data from 1990 to 2019, we identified possible RA births. We used at least 1 delivery-related ICD-9 or ICD-10-CM code and a validated RA algorithm requiring at least 1 ICD-9 (714*) or ICD-10-CM RA codes (M05*, M06.0, M06.2, M06.3, M06.8, M06.9), ever mention of a RA medication, and a RA keyword with a positive predictive value of 90%. RA cases were diagnosed by a rheumatologist, and we included pregnancies that occurred after RA diagnosis. We assessed seropositivity, age at RA diagnosis, and presence of erosive RA based on keyword search of notes and radiology reports. Medication use was defined as ever use during the pregnancy and at time of delivery. We assessed maternal and fetal outcomes with preeclampsia diagnosed by an obstetrician. Maternal peripartum outcomes included rates of blood transfusion, rates of infection at up to 6 weeks postpartum as defined by a clinician, and length of hospital stay in days.
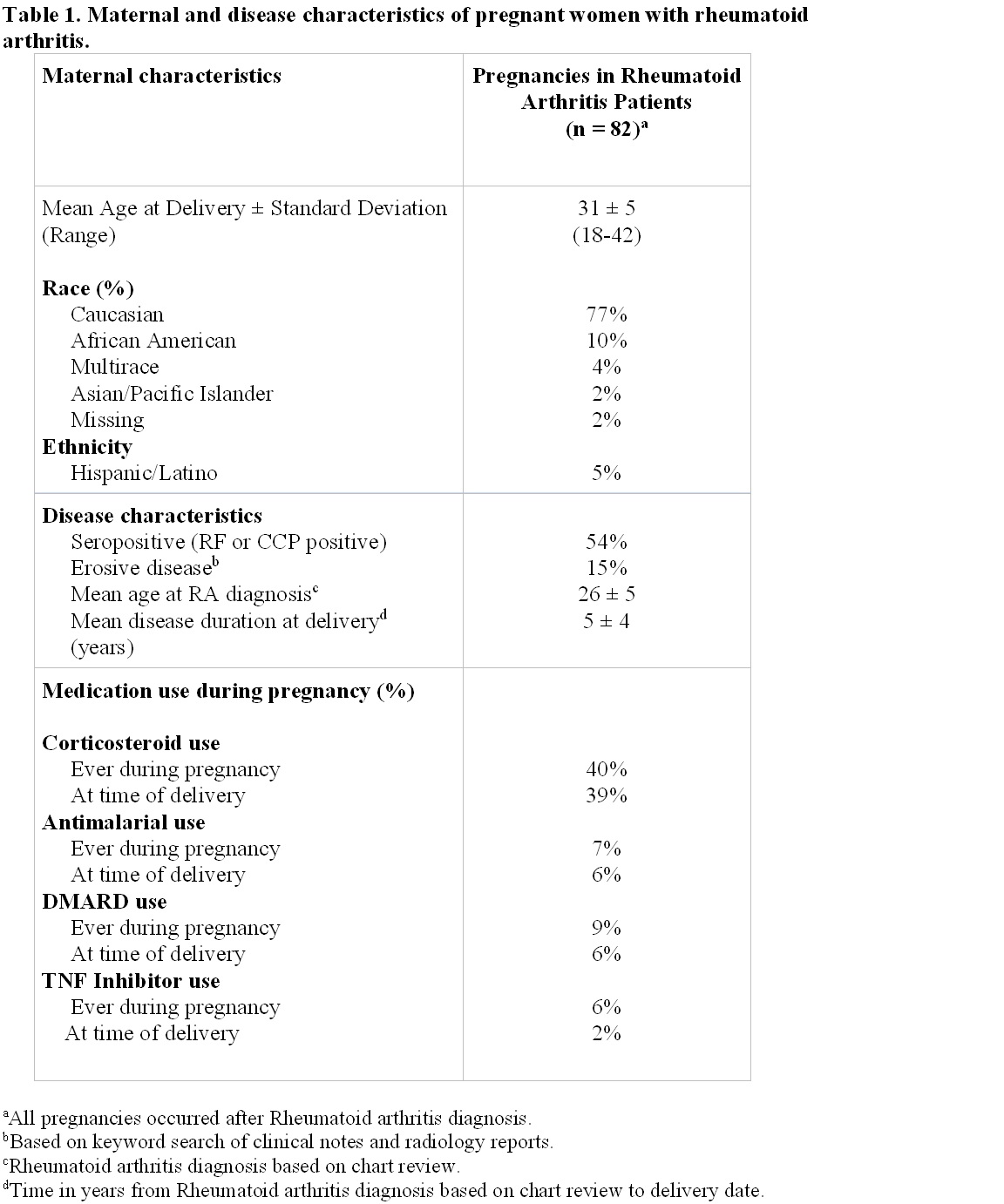
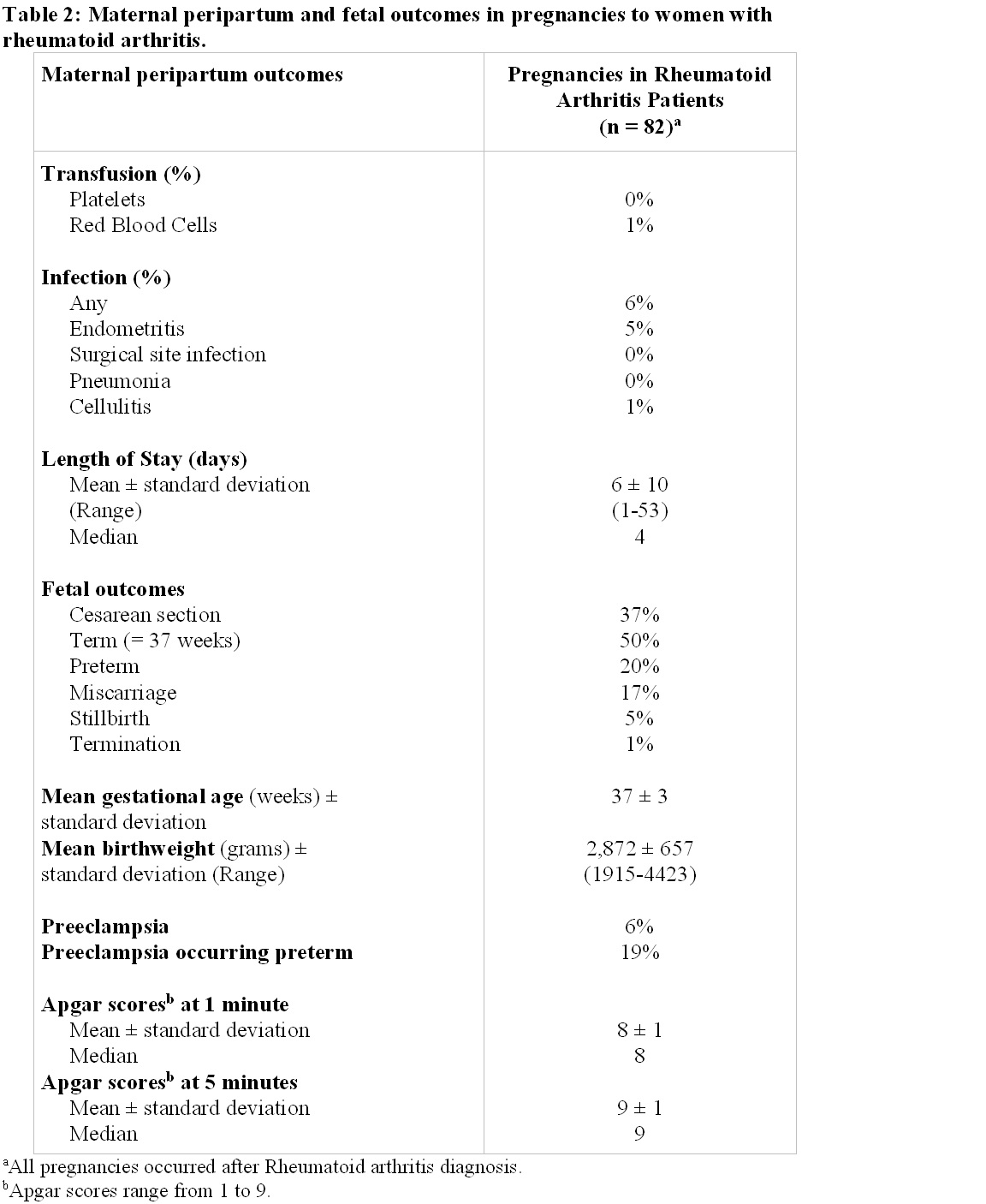
Results: We identified 82 pregnancies that occurred after RA diagnosis. Our RA cohort was predominantly White (77%) with 54% being seropositive and 15% having erosive disease (Table 1). Prednisone use ever during pregnancy and at the time of delivery was common (40% and 39%, respectively). Disease modifying anti-rheumatic drugs (DMARDs) and tumor necrosis factor inhibitor (TNFi) use during pregnancy were low (9% and 6%) with only 16% of pregnancies occurring before the first TNFi approval. For most cases, TNFis were discontinued prior to delivery. Rates of preterm delivery were higher than the general population (20% vs. 10%) but similar to rates in other RA studies (15-20%). Rates of preeclampsia (6%) and caesarean section (39%) for our cohort were no different than the general population and were similar to other RA studies (Table 2). Overall, infection rates were low with only 5 pregnancies (6%) having any infection. Of these 5 pregnancies with infection, 4 had endometritis and 1 cellulitis with no surgical site infections. In our cohort, the rate of peripartum red blood cell transfusions was 1%, which was similar to the general population. Median length of stay of 4 days was similar to the general population.
Conclusion: We identified pregnancies to RA mothers in a real-world, large EHR cohort. Corticosteroid use was common during pregnancy and at the time of delivery while DMARD and TNFi use was rare. Women with RA were at increased risk for preterm birth but had rates of preeclampsia and caesarean section similar to the general population. Compared to the general population, women with RA also had similar rates of peripartum infection and transfusions.
To cite this abstract in AMA style:
Tarplin S, Camai A, Barnado A. Maternal Peripartum Outcomes Are Similar to the General Population in Rheumatoid Arthritis Pregnancies [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/maternal-peripartum-outcomes-are-similar-to-the-general-population-in-rheumatoid-arthritis-pregnancies/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/maternal-peripartum-outcomes-are-similar-to-the-general-population-in-rheumatoid-arthritis-pregnancies/