Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Treatment of Rheumatoid Arthritis (RA) has changed drastically in the last two decades in strategies and objectives, as well as in therapeutic options, especially with the use of the disease modifying drugs (DMARD), both synthetic and biological. The data on the management of these patients under clinical trial conditions are abundant but it is necessary to expand our knowledge on how to use them in daily clinical practice. Purpose: to describe the clinical management and treatment in a cohort of patients with incident RA on daily clinical practice.
Methods: We conducted an observational longitudinal study. Patients: all recent onset RA diagnosed between January 1st 2007 and December 31st 2015 followed in outpatient clinic at Hospital Clinico San Carlos until January 1st 2017, which used any DMARD (synthetic and biologic) during at least 3 months. Variables: sociodemographic (age and gender), clinical (comorbidities, smoking status, date of diagnosis), quality of life (Rosser index), laboratory test (ESR, Rheumatoid Factor, ACPA), disease activity (HAQ and DAS28), treatments during follow-up (NAIDs, corticoids, DMARD (type, dates of start and discontinuation)) and treatment course (first or subsequent). Descriptive techniques were used of sociodemographic, clinical and treatment characteristics.
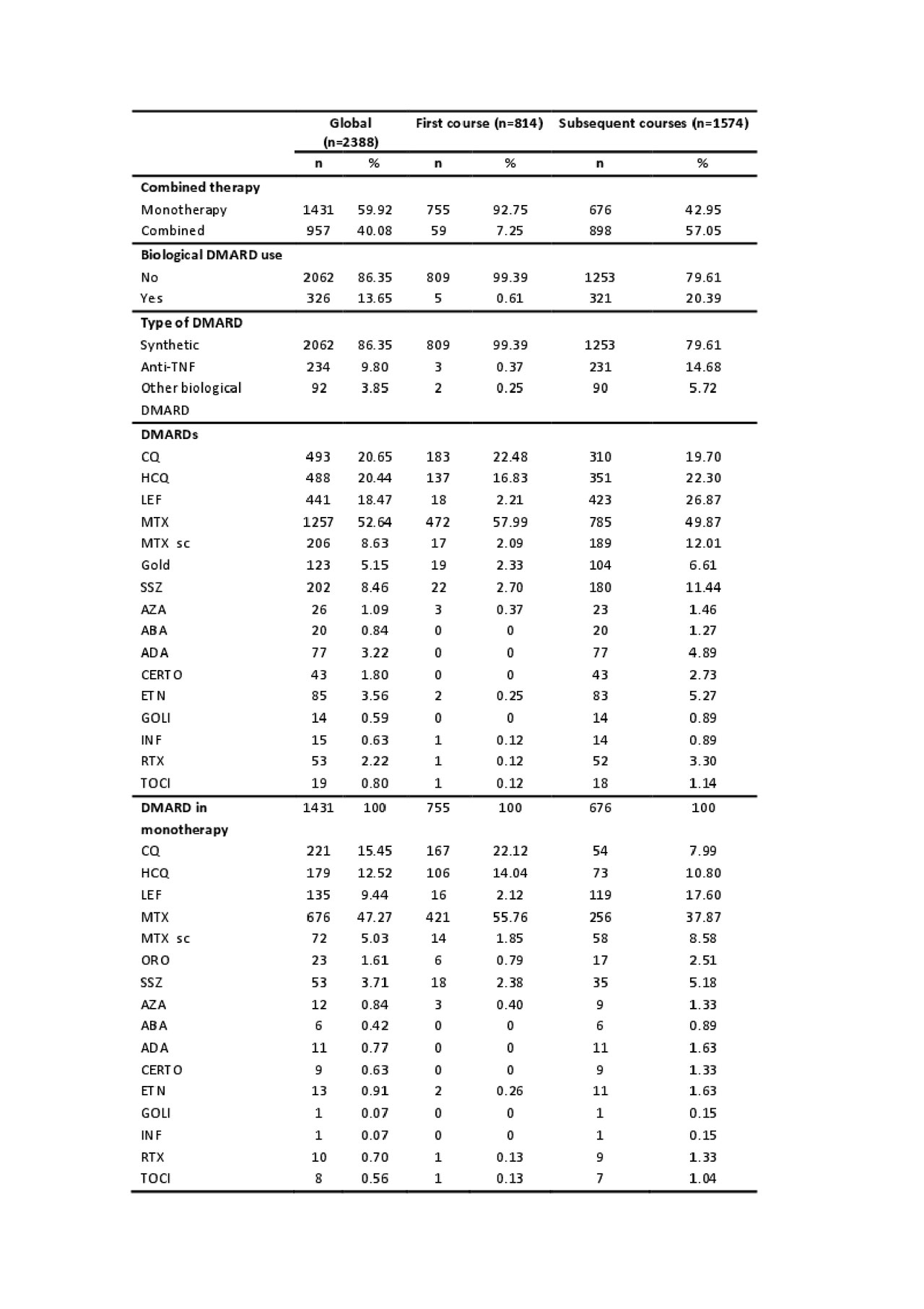
Results: We included 2388 courses of DMARD treatment in 814 patients. 77.52% were women with a mean age at diagnosis of 57.53±15.50 years. 63% of them were married and 85% lived with family. 44% had primary studies and 50% were in an active employment situation. The mean time to diagnosis was 8.8±226.3 months with a diagnosis in first visit in 72.9% of patients. 16% of patients were active smokers. The most frequent basal comorbidities were: hypertension (34%), dyslipidemia (30%), diabetes mellitus (13%) and depression (8.7%). The mean quality of life at the beginning of the disease measured by the Rosser index was 0.97 ± 0.04. 55% of patients were Rheumatoid Factor positive, 44% ACPA positive with a high mean DAS28 at the beginning of the disease (5.26±1.4). In table 1 we present all treatments globally and by treatment course. The mean time to the first treatment course was 21 [0-43] days.
Conclusion: Our patients have a poor quality of life at the beginning of the disease and present a severe activity. The management we do is aggressive and early with a diagnosis at first visit in 72.9% of patients. In 25% of patients treatment is prescribed from the moment of diagnosis and at least 50% of our patients are treated before a month from first visit. Most patients start with monotherapy, the frequency of combined treatment increases later on and it is more frequent after the second course of treatment. Methotrexate alone or in combination is the most frequently prescribed treatment. The use of biological DMARD increases throughout the follow-up, the most frequent being Adalimumab. The preferred combinations by our rheumatologists are Methotrexate – Antimalarial, Methotrexate – Leflunomide and Methotrexate – Adalimumab.
To cite this abstract in AMA style:
Hernandez Rodriguez i, Rosales Rosado Z, Lois p, Lajas C, Font Urgelles J, Jover Jover J, Abasolo Alcazar l. Management of Patients with Incident Rheumatoid Arthritis in Rheumatology Clinical Practice [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/management-of-patients-with-incident-rheumatoid-arthritis-in-rheumatology-clinical-practice/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/management-of-patients-with-incident-rheumatoid-arthritis-in-rheumatology-clinical-practice/