Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Most data on management and outcomes of ANCA-associated vasculitis (AAV) come from highly selected populations in tertiary referral centres, or clinical trials. These results may not be generalizable to clinical practice across all hospitals.Methods:
Rheumatology and Renal units in all hospitals within one of four health regions in England were invited to undertake a retrospective case note audit of all patients newly diagnosed with AAV during April 2013-December 2014. Data were collected on specialty of attending physician, patient demographics, place of diagnosis, date of symptom onset, admission or first clinic appointment, and diagnosis, BVAS organ systems involved, details of remission induction, and outcomes including hospitalisation for infection and death. The odds ratio (OR) for infection was estimated using logistic regression, and the hazard ratio (HR) for death was estimated using cox regression; both were adjusted for confounders age and renal involvement.Results:
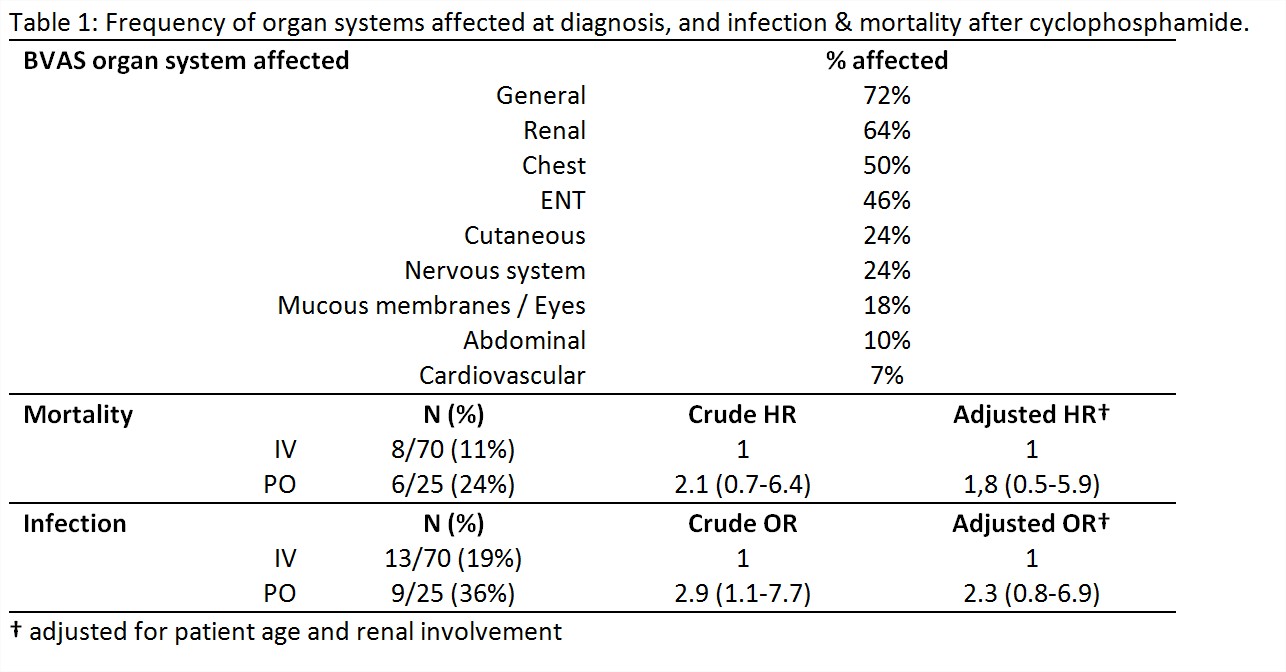
Cases were contributed by 19 (56%) of 34 invited units. 126 newly diagnosed cases were included, 59% from Rheumatology and 41% from Renal units. 69 (54.8%) were diagnosed as inpatients, and 57 (45.2%) as outpatients. Cyclophosphamide (CYC) was the most common remission agent used in 95 (75%), Rituximab in 6 (5%), and other agents in 25 (20%). Frequency of organ involvement at diagnosis is shown in table 1. Diagnostic delay from first symptoms to diagnosis was median 2.6 (interquartile range 1.2-6.1) months. It was shorter in the sicker patients (defined as inpatients) 1.8(0.9-3.7) compared to outpatients, 4.1(2.0-12.6). Among inpatients, delay from admission to diagnosis ranged from 0-53 days (median 6, IQR 3-10.5). Of the 95 newly diagnosed patients treated with CYC, 70 (74%) received IV and 25 (26%) oral. 22 (23%) had infections requiring hospitalisation during or within 6 months of CYC treatment, and 14 (15%) died during follow up (table 1). Compared to IV, the crude OR for infection with oral CYC was 2.9 (1.1-7.7) and HR for death was 2.1 (0.7-6.4). Once adjusted for age and renal involvement, OR for infection remained elevated at 2.3 (0.8-6.9) and HR for death was 1.8(0.5-5.9).Conclusion:
There are potential opportunities to reduce the delay between admission and diagnosis amongst hospitalised patients. The need to improve care is highlighted by the significant mortality and infection rate in this unselected group. Although this analysis is limited by lack of power, and like all observational comparison of treatments at risk of confounding by indication, it raises the hypothesis that in contrast to the more selected CYCLOPS trial population, the routine use of oral CYC may be associated with an increased risk of death and infection requiring hospitalization.
Disclosure: F. Pearce, None; C. McGrath, None; R. Sandhu, None; J. Packham, None; K. Obrenovich, None; R. A. Watts, None; P. Lanyon, None.
To cite this abstract in AMA style:
Pearce F, McGrath C, Sandhu R, Packham J, Obrenovich K, Watts RA, Lanyon P. Management and Outcomes of ANCA-Associated Vasculitis in Unselected Cases within a Large Health Region of England [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/management-and-outcomes-of-anca-associated-vasculitis-in-unselected-cases-within-a-large-health-region-of-england/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/management-and-outcomes-of-anca-associated-vasculitis-in-unselected-cases-within-a-large-health-region-of-england/