Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Knee OA is often accompanied by loss of passive extension, termed a flexion contracture (FC), resulting in worse clinical outcomes. To our knowledge, MRI-based studies examining OA-related changes associated with knee FC have not been performed. Our objective was to study associations between knee FC and MRI-based OA-related structural changes. We hypothesized: 1) knee FC would be associated with cartilage lesions and bone marrow lesions (BMLs) in the patellofemoral (PF) joint, as well as osteophytes and meniscal alterations, and 2) normal knee extension would have high negative predictability for PF cartilage lesions and BMLs. We tested our hypotheses using data from the Osteoarthritis Initiative (OAI).
Methods: The OAI (NCT00080171, ethics approval #10-00532) is a National Institutes of Health (NIH)-funded, multi-center, prospective cohort study focusing on knee OA. For this study, 596 knees with knee extension data from the Foundation for the NIH nested case-control study were included. Knee extension was measured with a goniometer using a method with high inter-rater reliability. Inability to extend the knee to 0° constituted a FC.
Enrolment 3-Tesla MRI images were scored with the MRI Osteoarthritis knee score (MOAKS) system with assessors blinded to participant ID. Structural changes (cartilage lesions, BMLs, osteophytes, meniscal alterations, effusion, synovitis) within MOAKS-based regions of the knee that could biomechanically obstruct extension were analyzed (Figure 1A). Multivariable linear regression models evaluated for effect size of MRI outcomes on knee extension. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) were calculated based on presence or absence of FC. Area under the curve (AUC) was calculated using knee extension as a continuous variable for all participants and those without radiographic OA [Kellgren-Lawrence (KL) scores 0-1] or knee hyperextension.
Results: Of 596 participants, 72 (12.1%) had KL scores 0-1 (3.9% FC, 8.2% no FC). Knee alignment was overall 0.3±3.7° valgus. Higher lateral femoral cartilage scores (indicating greater size and depth of cartilage lesions on the femoral side of the lateral PF joint) and BML number scores were associated with lost knee extension (Table 1). Higher osteophyte scores in multiple regions correlated with lost knee extension (Table 1). Worse meniscal score in the medial meniscal body and posterior horn and a worse effusion score correlated with lost knee extension (Table 1). A representative image of a knee with FC is shown in Figure 1B.
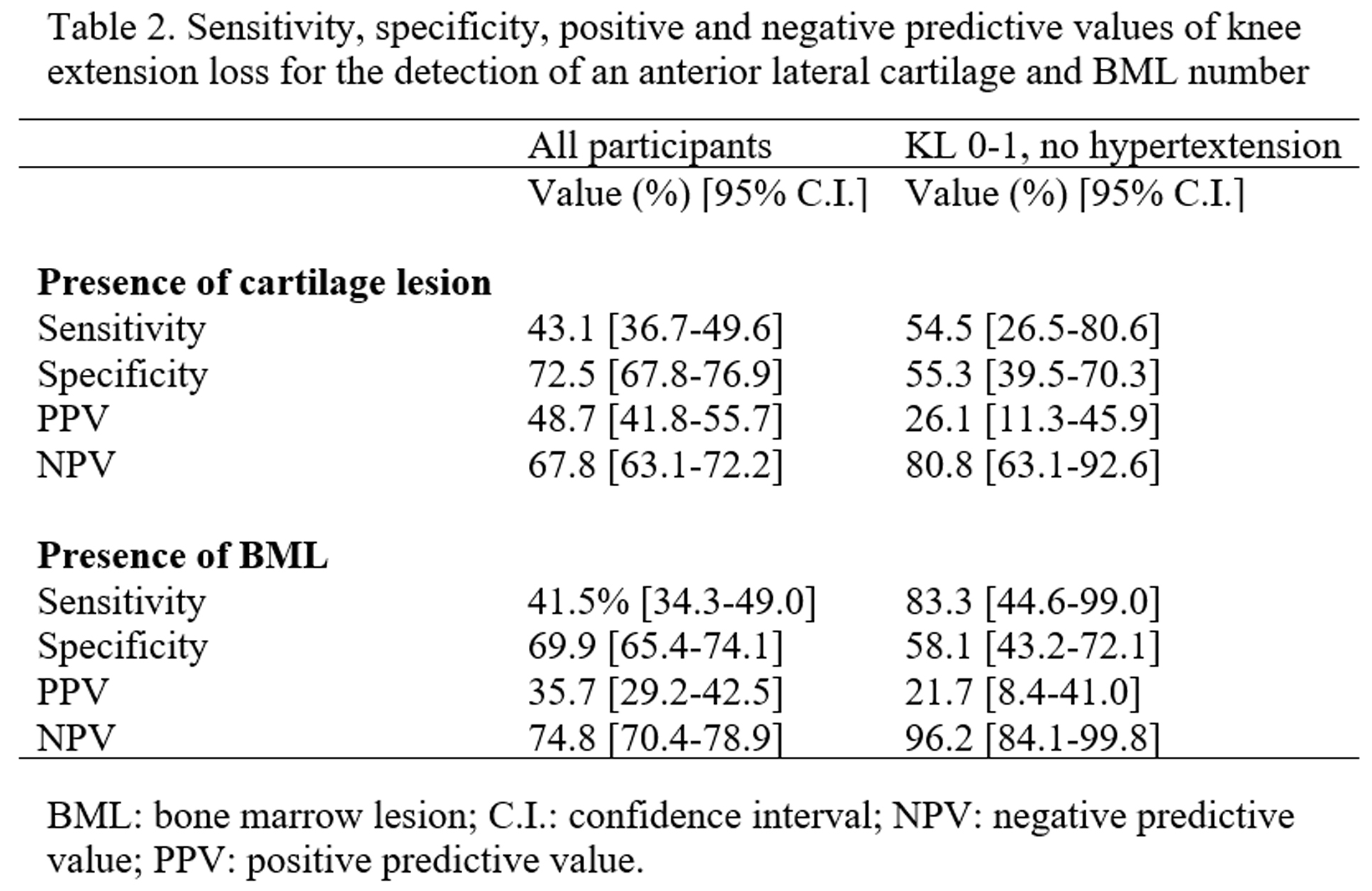
Sensitivity, specificity, PPV and NPV for presence/absence of knee FC are summarized in Table 2. For those with KL score 0-1 without hyperextension AUC was 0.77 (95% C.I. 0.55-0.98; Figure 1C).
Conclusion: Knee extension loss was associated with widespread degenerative changes, including those not visible on knee x-ray, and appears to be linked to global severity of disease. Precisely measuring knee extension may help predict knee OA progression, obviating the need for MRI and reducing health care costs. Longitudinal studies evaluating knee extension as a biomarker for MRI-related structural changes are needed.
 Figure 1. Structural changes associated with knee extension loss. (A) Left: Regional knee division of the MRI Osteoarthritis Knee Scoring system. Cartilage and bone marrow lesions were evaluated in the patellar, anterior (ant) and middle (mid) femoral, and anterior tibial regions where they could limit knee extension via pain inhibition. Osteophytes were evaluated in the patellar, anterior and middle femoral and anterior tibial regions where they could mechanically limit knee extension. Meniscal lesions were evaluated in all regions, as any “locking” from meniscal tears could limit knee extension. Right: Corresponding coronal sections where medial and lateral regions were investigated. (B) MRI of a participant with knee flexion contracture Left: Dual echo steady state sequence showing thinner articular cartilage in the antero-lateral femur making up the femoral side of the patellofemoral joint (arrowhead) and patellar osteophytes (arrows). Right: T2-weighted image with bracket showing large BML in the antero-lateral femur. (C) Receiver-operator curves for the presence of cartilage lesion (left) and bone marrow lesion (BML, right). Top: All participants KL 0-1 (n=596). Bottom: KL 0-1, excluding knees with hyperextension (n=49). Ant: anterior; AUC: Area under the curve; Med: medial; Lat: lateral; Mid: middle; Pos: posterior.
Figure 1. Structural changes associated with knee extension loss. (A) Left: Regional knee division of the MRI Osteoarthritis Knee Scoring system. Cartilage and bone marrow lesions were evaluated in the patellar, anterior (ant) and middle (mid) femoral, and anterior tibial regions where they could limit knee extension via pain inhibition. Osteophytes were evaluated in the patellar, anterior and middle femoral and anterior tibial regions where they could mechanically limit knee extension. Meniscal lesions were evaluated in all regions, as any “locking” from meniscal tears could limit knee extension. Right: Corresponding coronal sections where medial and lateral regions were investigated. (B) MRI of a participant with knee flexion contracture Left: Dual echo steady state sequence showing thinner articular cartilage in the antero-lateral femur making up the femoral side of the patellofemoral joint (arrowhead) and patellar osteophytes (arrows). Right: T2-weighted image with bracket showing large BML in the antero-lateral femur. (C) Receiver-operator curves for the presence of cartilage lesion (left) and bone marrow lesion (BML, right). Top: All participants KL 0-1 (n=596). Bottom: KL 0-1, excluding knees with hyperextension (n=49). Ant: anterior; AUC: Area under the curve; Med: medial; Lat: lateral; Mid: middle; Pos: posterior.
To cite this abstract in AMA style:
Campbell T, Trudel G, McGonagle D. Magnetic Resonance Imaging Structural Changes Correlated with Knee Extension: Data from the Osteoarthritis Initiative [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/magnetic-resonance-imaging-structural-changes-correlated-with-knee-extension-data-from-the-osteoarthritis-initiative/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/magnetic-resonance-imaging-structural-changes-correlated-with-knee-extension-data-from-the-osteoarthritis-initiative/