Session Information
Date: Monday, November 11, 2019
Title: 4M096: Spondyloarthritis Including Psoriatic Arthritis – Clinical III: Miscellaneous (1818–1823)
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Prevalence of sacroiliitis (SI) in Crohn’s disease (CD) varies widely (range 4% -39%), depending on criteria utilized to define the disease (e.g. inflammatory back pain, plain radiographs or MRI). Sacroiliitis may remain underdiagnosed in CD patients given lack of association with clinical symptoms of back pain and CD activity. However, patients with CD often undergo magnetic resonance enterography (MRE) to assess extent, severity of small bowel CD and radiographic healing, affording clinicians the opportunity to evaluate for the presence of active and/or chronic SI. We sought to identify the prevalence of sacroiliitis in CD patients utilizing MRE and determine its relationship with CD activity, especially with concurrent biologic therapy.
Methods: All CD subjects undergoing MRE between years 2014-2018 at a large IBD referral center were identified. A musculoskeletal radiologist, blinded to clinical data, reviewed all MRE exams for the presence of acute bone marrow edema (BME) lesions and chronic lesions suggestive of acute and chronic SI, respectively. A second radiologist, also blinded, assessed MRE for mucosal CD activity using validated measures. Charts were reviewed for demographics, IBD characteristics, presence of back pain, clinical and endoscopic activity of CD, and Crohn’s therapies within 3 months of MRE. Comparisons were made between CD subjects with and without SI using chi-square test. Univariate and multivariate logistic regression were used to determine risk factors of SI.
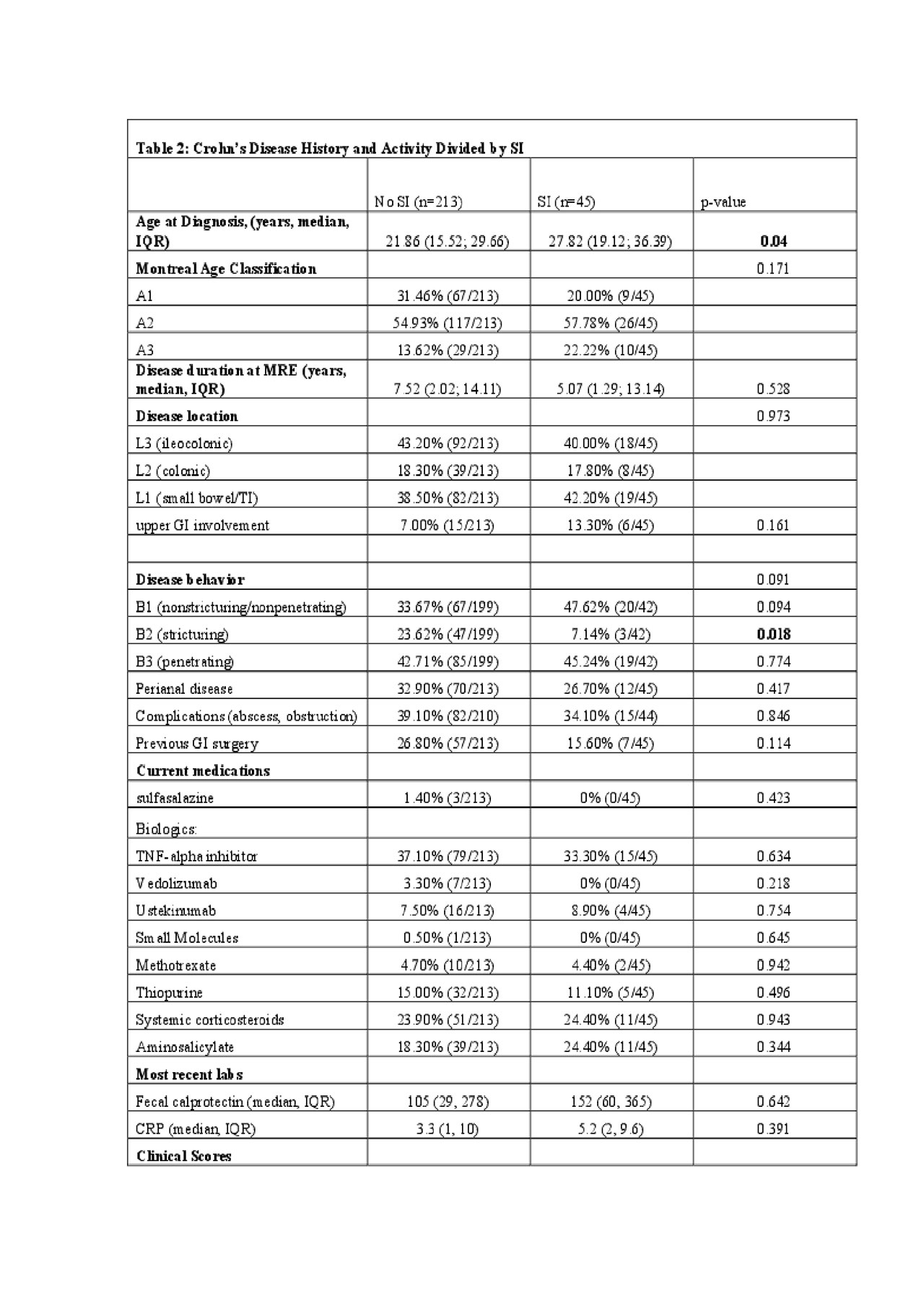
Results: 258 subjects with CD underwent MRE during the study period with a mean age of 35 years old, 53% (n=138) were male, and mean duration of CD at the time of MRE was 9 years. Few reported back pain (8%) and 14% had previously seen a rheumatologist. Overall, 17% (n=45) of patients had MR evidence of sacroiliitis (Table 1). Female gender, presence of back pain, and later age of CD diagnosis were associated with signs of sacroiliitis (p=0.05, p< 0.001, p=0.04 respectively; Table 2). Stricturing phenotype was associated with a lower rate of SI (7% vs. 24%; p=0.018), but inflammatory or penetrating phenotypes were not. CD location, activity as noted by clinical scores, endoscopic disease activity, or radiographic disease activity on MRE, were not associated with sacroiliitis (Table 2). On multivariable analysis, back pain was associated with the presence of sacroiliitis on MRE (OR 3.0, 95% CI 1.1- 5.6; p=0.04). Concurrent CD therapy with biologics did not lower the risk of sacroiliitis.
Conclusion: Although often underdiagnosed, SI is a common comorbid condition in CD. While recent history of back pain was associated with the presence of sacroiliitis visualized on MRE, no correlations were found with other clinical and endoscopic markers of CD activity. Moreover, concurrent CD therapy, especially biologics, was not associated with a lower risk of sacroiliitis on MRE. With limited clinical clues and CD characteristics to suggest sacroiliitis, gastroenterologists can utilize MRE as a screening tool to detect SI and refer CD patients to rheumatologists. Presence of SI on MRE in CD patients with back pain may help identify a subset of individuals likely to benefit from switching to therapies with proven efficacy in axial SpA.
To cite this abstract in AMA style:
Malik F, Levine I, Castillo G, Jaros B, Alaia E, Ream J, Axelrad J, Hudesman D, Scher J. Magnetic Resonance Enterography as a Screening Tool to Detect Sacroiliitis in Crohn’s Disease: Association with Clinical and Endoscopic Markers of Crohn’s Disease Activity [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/magnetic-resonance-enterography-as-a-screening-tool-to-detect-sacroiliitis-in-crohns-disease-association-with-clinical-and-endoscopic-markers-of-crohns-disease-activity/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/magnetic-resonance-enterography-as-a-screening-tool-to-detect-sacroiliitis-in-crohns-disease-association-with-clinical-and-endoscopic-markers-of-crohns-disease-activity/