Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: SLE, primary Sjögren’s disease (pSjD) and APS are systemic rheumatic diseases (SRD) that mainly affect women of childbearing age and have been associated with adverse pregnancy outcomes (APO). This study aims to identify immunological imbalances in placentas from patients with SLE, pSjD or APS, focusing on IFN and immune cell subsets compared to placentas of healthy pregnancies and of APO of women without these SRD.
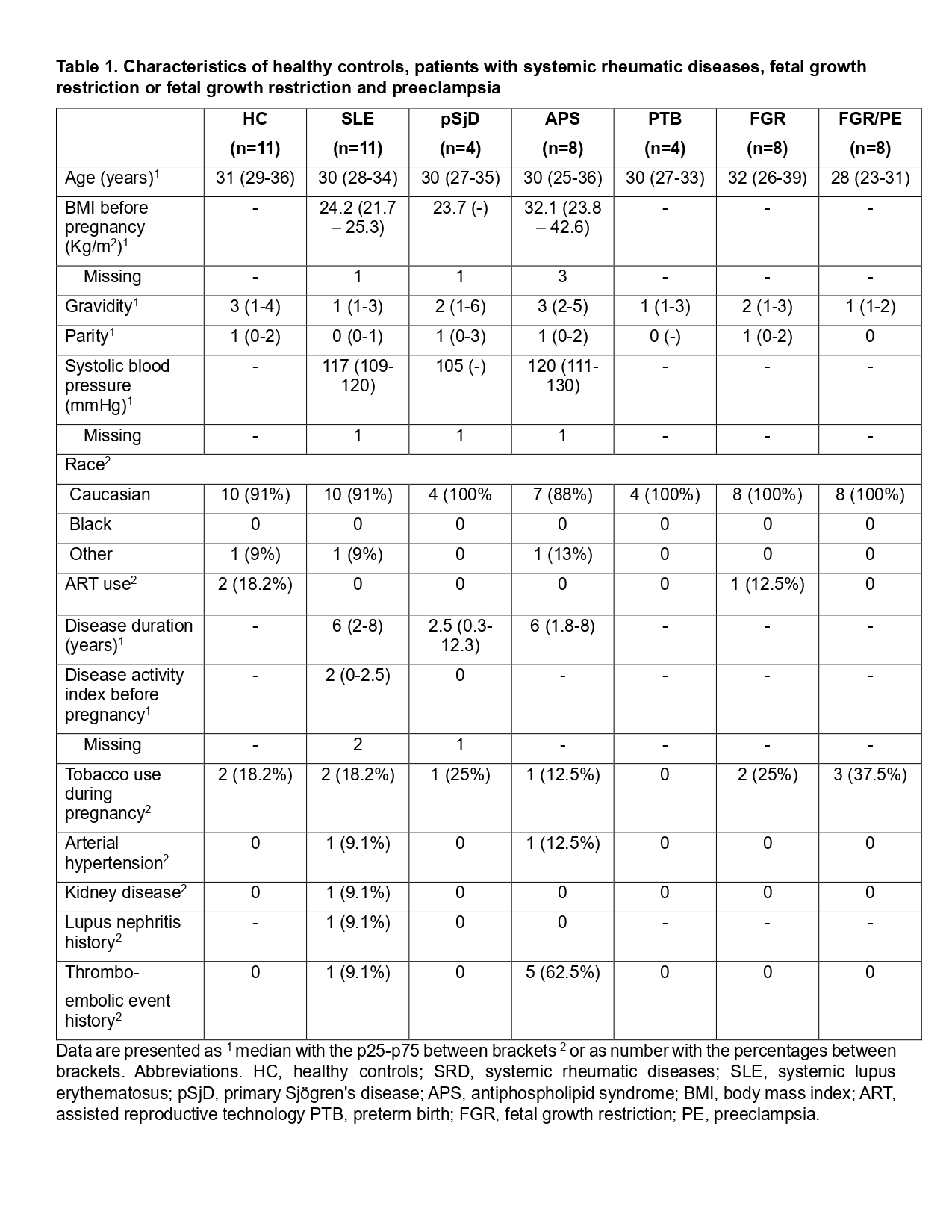
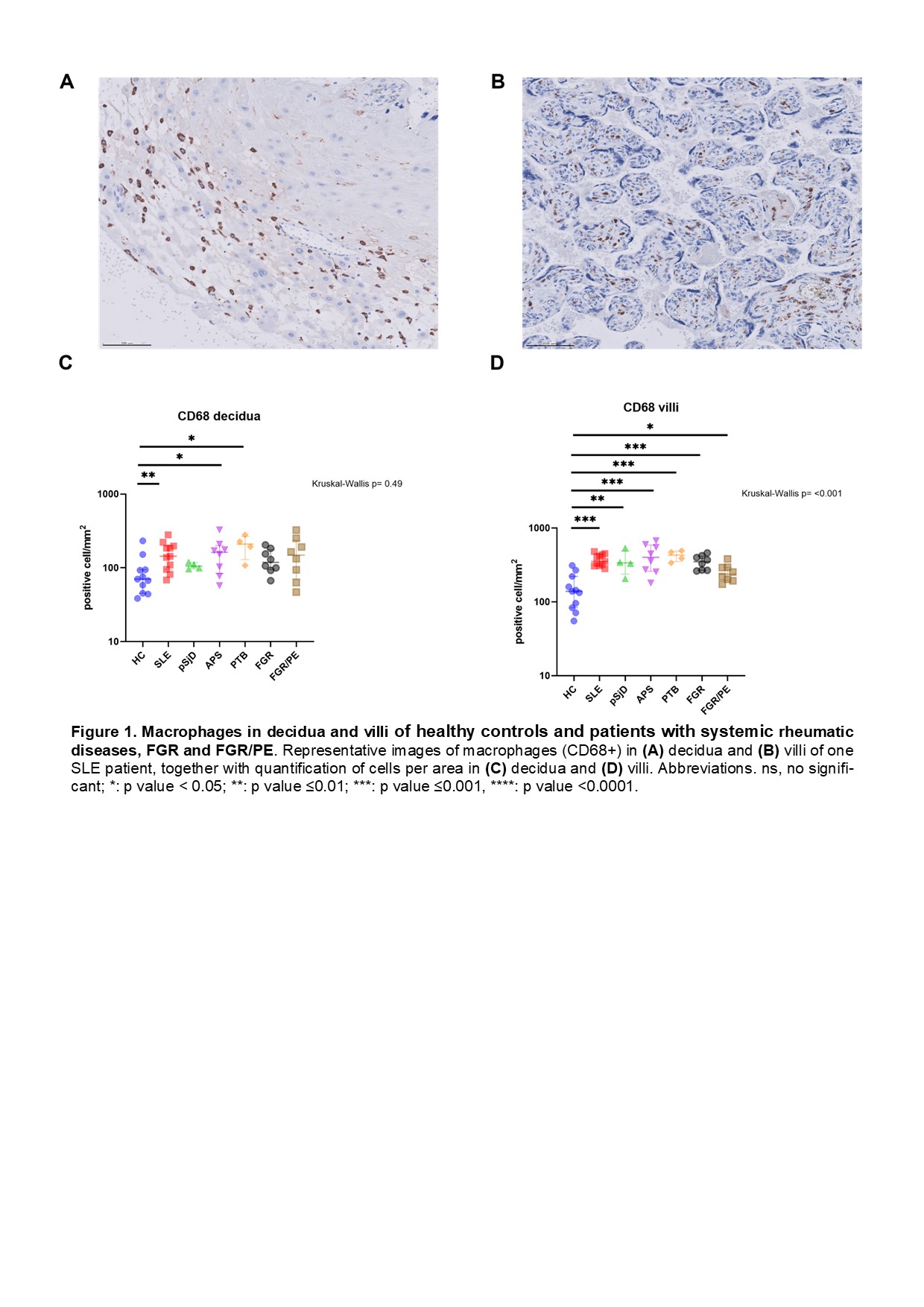
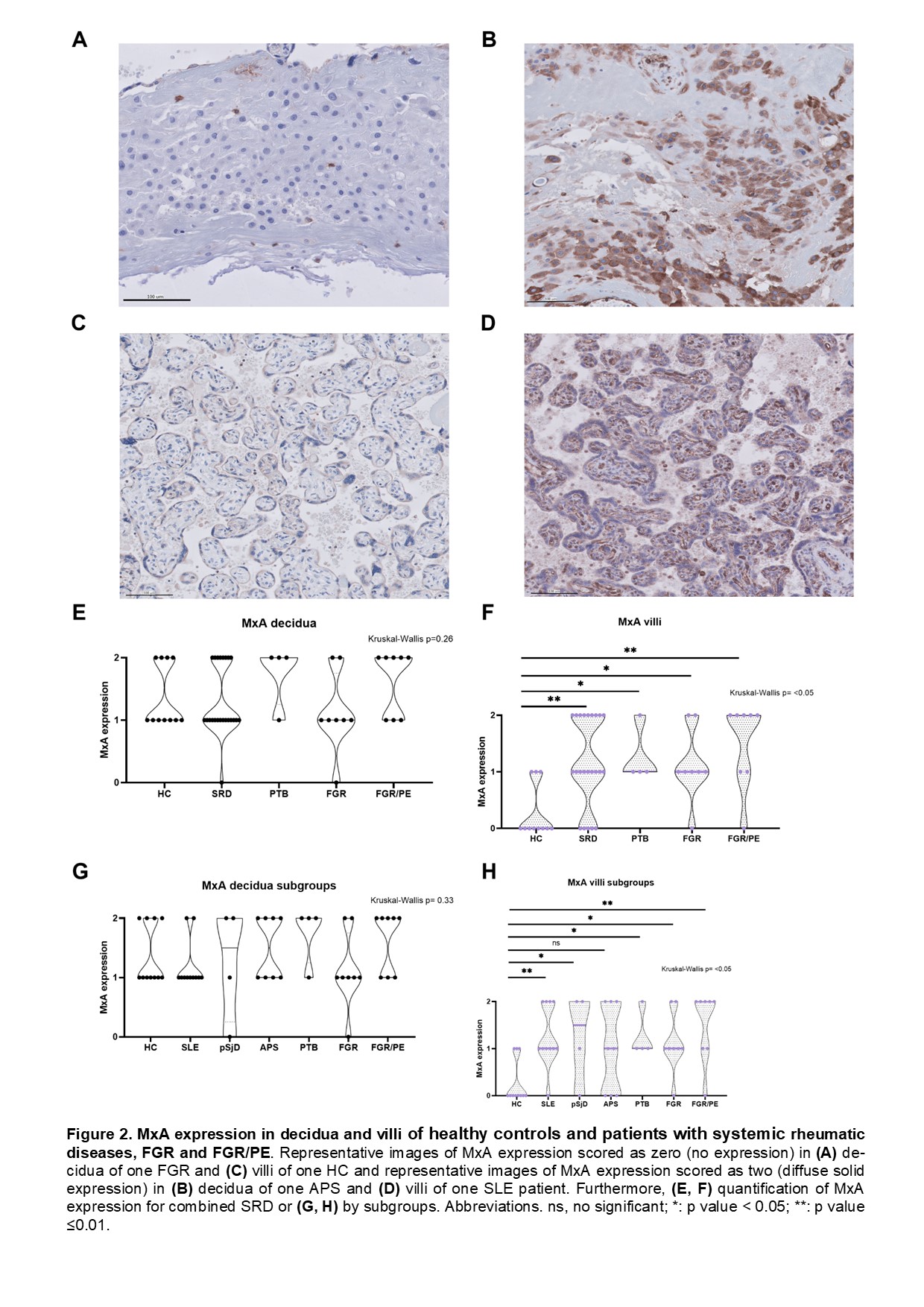
Methods: Placenta biopsies from healthy controls (HC), SLE, pSjD, APS and control patients with fetal growth restriction (FGR), preterm birth (PTB), or FGR and preeclampsia (FGR/PE) were recovered from the pathology biobank at our university hospital. Clinical characteristics and APO were retrieved from medical records. APO were defined as the presence of PTB, FGR, PE or thromboembolic events during pregnancy or postpartum. Immunohistochemistry was performed for Myxovirus resistance protein 1 (MxA), CD3, CD20, CD56, CD68, and CD123. The proportion of positive cells was established using an automated detection classifier, while MxA expression was assessed semi/quantitatively discriminating between maternal (decidua) and fetal (villi) tissue. Finally, placental lesion classification was performed according to the Amsterdam Workshop Group recommendations.
Results: Our study included placentas from 11 SLE, 4 pSjD, 8 APS, 8 FGR, 8 FGR/PE patients and 11 HC. Demographic and disease characteristics before pregnancy are summarized in Table 1. Patients with SRD had a high rate of APO (70%). The most common APO in SLE patients was PTB (54.5%), followed by FGR (27.3%), while APS patients had high rates of PTB (75%) and PE (63%). SRD patients had higher macrophage (CD68+) counts in decidua and villi than HC as depicted in Figure 1. In decidua, this difference was found in the placentas of SLE and APS patients, while in villi, pSjD patients also had higher macrophage counts. Concerning patients without SRD, in decidua, only PTB showed an increase macrophage count compared to HC. In villi, this difference was significant for PTB, FGR and FGR/PE patients. No differences were observed in T (CD3+), B (CD20+) and NK (CD56+) cells between patients with SRD and HC in decidua and villi, and no plasmacytoid dendritic cells (CD123+) were identified. Patients with SRD had higher MxA values than HC in villi but not decidua and this difference was explained by SLE and pSjD patients, while APS patients did not show significant differences with HC. PTB, FGR and FGR/PE groups were associated with a higher MxA expression in villi compared to HC, which was not the case for decidua tissue. Finally, placental lesions were frequently found in SRD patients, while SLE patients had a high prevalence of chorioamnionitis (CA) (55%), APS patients had higher rates of maternal vascular malperfusion (75%) and villitis of unknown etiology (38%).
Conclusion: SLE, pSjD and APS patients have an increased macrophage count and interferon upregulation in the placenta compared to HC. This upregulation seems to occur in the chorionic villi rather than the decidua. Therefore, a pro-inflammatory environment led by innate immune components seems to be the main cause of placental dysfunction and APO presentation.
To cite this abstract in AMA style:
Fierro J, Schoots M, Liefers S, Doornbos-van der Meer B, Diercks G, Bootsma H, Prins J, Westra J, de Leeuw K. Macrophages and Interferon Upregulation in Placentas from Patients with Systemic Lupus Erythematosus, Primary Sjögren’s Disease and Antiphospholipid Syndrome [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/macrophages-and-interferon-upregulation-in-placentas-from-patients-with-systemic-lupus-erythematosus-primary-sjogrens-disease-and-antiphospholipid-syndrome/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/macrophages-and-interferon-upregulation-in-placentas-from-patients-with-systemic-lupus-erythematosus-primary-sjogrens-disease-and-antiphospholipid-syndrome/