Session Information
Date: Friday, November 6, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Clinical Manifestations
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with SLE have poor health related quality of life (HRQoL), however the differences in the predominant causes of decreased HRQoL across subgroups of SLE are not known. Features of fibromyalgia including fatigue, widespread pain, depression, sleep and cognitive dysfunction are prevalent in SLE affecting 20-65% of patients and often contribute to disability and poor HRQoL. These aspects of fibromyalgia have not been well described in patients with lupus nephritis (LN). We evaluated self-reported symptoms of fibromyalgia and mood disorders in patients with and without lupus nephritis.
Methods: This was a cross sectional study of SLE patients (ACR 1997 or SLICC 2012 criteria) enrolled in a university registry from June 2018 to November 2019. All patients completed Systemic Lupus Activity Questionnaire (SLAQ), Patient Health Questionnaire-9 (PHQ9), and 2016 ACR Fibromyalgia criteria surveys. Active nephritis was defined as UPC >500mg and/or active urinary sediment excluding other causes. Fibromyalgia was defined as ≥7 widespread pain index (WPI) with ≥5 symptoms severity score (SSS) or ≥4 WPI with ≥9 SSS. Differences across groups were analyzed by Fisher’s exact test and ANOVA.
Results: Two hundred and twenty-four patients completed patient-reported outcome measures (93% female, mean age 40 years, 67% Black). In our cohort 11% had active nephritis, 35% had nephritis in remission and 54% had no history of nephritis. Of nephritis patients, 22% had membranous class V, 48% had proliferative or proliferative/mixed LN, 3% class I/II, 5% post-transplant, 6% ESRD on dialysis, and class was unknown in 28%.
Active nephritis patients were younger, more often of Black race, and reported greater social support than non-nephritis patients. There were no differences in sex, disease duration, education, income, disability, insurance, or serologies. The use of plaquenil, anti-depressants, gabapentinoids, muscle relaxers, and narcotics were similar between groups. Active nephritis patients were more often prescribed prednisone (Table 2).
The prevalence of fibromyalgia was 13% in active nephritis, 3% in nephritis remission and 21% in non-nephritis patients (p=0.001). LN patients had significantly lower fibromyalgia severity, symptom severity, areas of pain, fatigue, cognitive, and sleep dysfunction. Patient-reported disease activity was significantly lower in patients with LN remission. Rates of anxiety and depression were similar across active LN and non-nephritis groups.
Conclusion: Patients with active and inactive LN report less fatigue, fibromyalgia, sleep, and cognitive dysfunction compared to non-nephritis patients. There were differences in demographics as well as greater social support in nephritis patients. Differences in social support could potentially mitigate fatigue and fibromyalgia in nephritis patients. There was no difference in anxiety or depression, suggesting fibromyalgia can occur independently of mood disorders. The drivers of low HRQoL may be distinct across SLE subgroups. Lupus nephritis patients have high rates of disability and poor HRQoL; however, the mechanism underlying these outcomes is nephritis is less likely related to features of fibromyalgia.
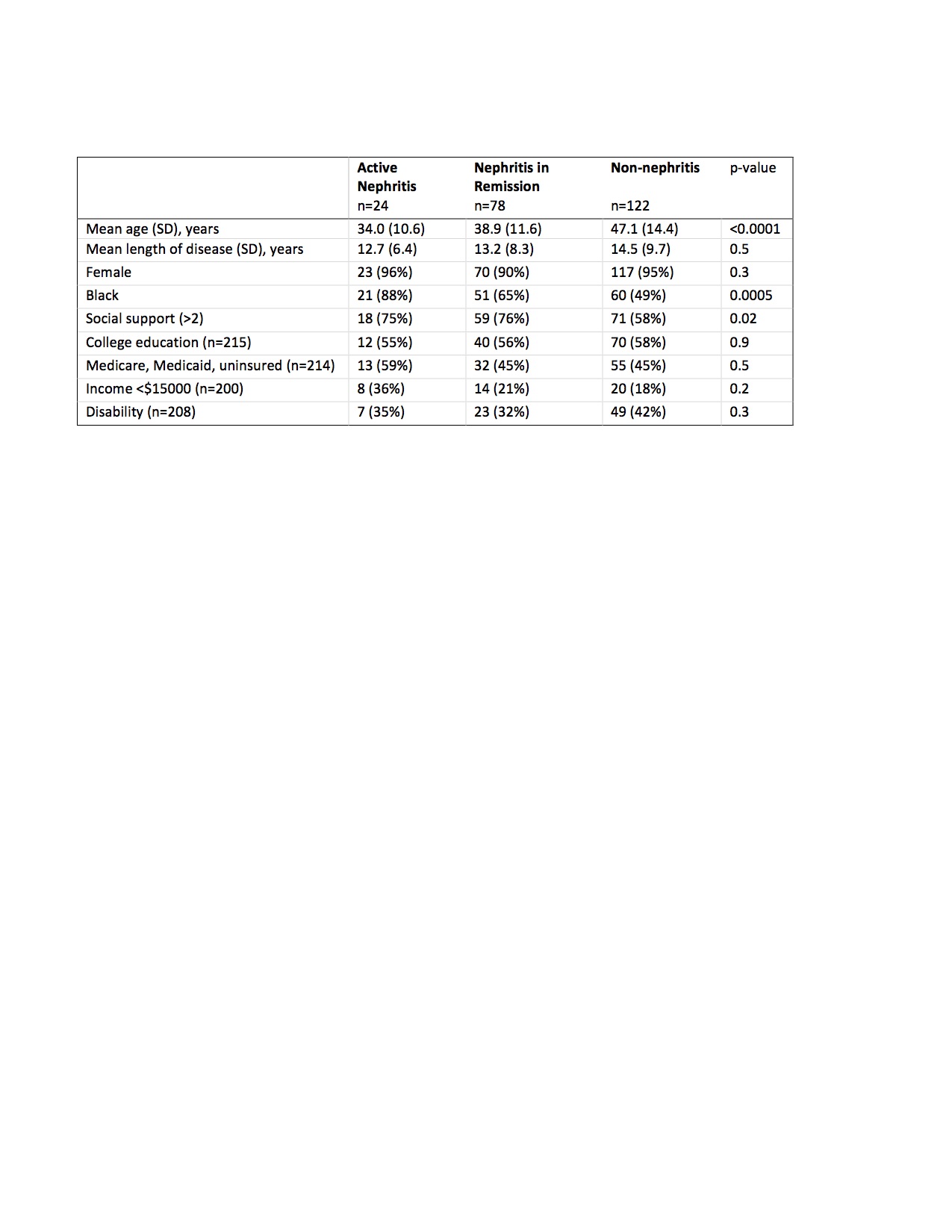 Table 1. Patient demographics and socioeconomic factors of active nephritis, nephritis in remission and non-nephritis SLE patients
Table 1. Patient demographics and socioeconomic factors of active nephritis, nephritis in remission and non-nephritis SLE patients
 Table 2. Physician- and patient-reported measures in active nephritis, nephritis in remission and non-nephritis SLE patients
Table 2. Physician- and patient-reported measures in active nephritis, nephritis in remission and non-nephritis SLE patients
To cite this abstract in AMA style:
Rogers J, Clowse M, Criscione-Schreiber L, Doss J, Sadun R, Sun K, Eudy A. Lupus Nephritis Is Associated with a Reduced Prevalence of Fibromyalgia [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/lupus-nephritis-is-associated-with-a-reduced-prevalence-of-fibromyalgia/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lupus-nephritis-is-associated-with-a-reduced-prevalence-of-fibromyalgia/
