Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Black, Hispanic, and Native American populations in the US experience increased morbidity and mortality from systemic lupus erythematosus (SLE), with higher rates and worse outcomes for lupus nephritis (LN). The purpose of our study was to identify socio-demographic indicators and outcomes of lupus nephritis on a national level in order to identify disparities and potential areas for intervention.
Methods: Our study utilizes the National Inpatient Sample (NIS), which is an all-payer national database. We used the NIS to identify inpatient hospitalizations between October 2015 and December 2017 with an ICD-10 diagnosis of SLE stratified by the additional diagnosis of lupus nephritis (LN) in patients 18 or older. We calculated the rate of lupus nephritis during hospitalizations, organized by patient and facility demographics. In addition, we examined dialysis, death, and cost of care for SLE and LN hospitalizations.
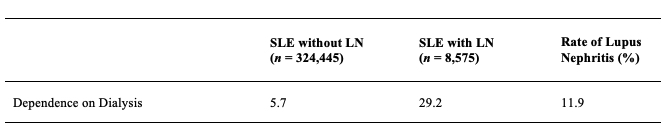
Results: We identified 333,020 hospitalizations with SLE, of which 8,575 (2.6%) included an LN diagnosis. The median age was lower LN group compare to SLE patients without LN (37 vs 55 years, p < .001) (Table 1). SLE disproportionately affects females, however, the lupus nephritis rate was higher in males than females (3.8 vs. 2.4). Hospitalizations with SLE were disproportionately higher in the White population, Black cohort (28.1%) and relatively lower in the Hispanic cohort (11.6%) Rates of LN were higher for Blacks (4.6%), Hispanics (4.0%) and Other races (3.7%) compared to Whites (1.1%, all p < .001). The lowest income quartile had the highest rate of LN (3.0%) and the upper quartile the lowest (2.1%, p < .001). Discharge with dialysis- dependence occurred in 29% of hospitalizations with LN diagnoses (Table 2). Cost of hospitalization was significantly higher with LN than without LN ($11,200 vs. $9,109, p < .001) (Table 3).
Conclusion: From the NIS hospitalizations, the presence of LN among hospitalizations with SLE is disproportionately associated with younger populations, Black and Hispanic populations and lowest income quartile. These hospitalizations primarily occur at urban teaching hospitals. There was a significant increase in cost associated with these hospitalizations. The rate of LN and dialysis is particularly concerning given the younger age of these hospitalizations. Further investigation is essential for identifying the structural causes that leads to these disparities and informing equitable care for patients with SLE and LN.
To cite this abstract in AMA style:
Gupta S, Willer K, Begovic A, Waters M, Tarantino L, Badejo O, Walters R, Townley T. Lupus Nephritis Disparities Amongst Hospitalizations in the United States: A National Inpatient Sample Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/lupus-nephritis-disparities-amongst-hospitalizations-in-the-united-states-a-national-inpatient-sample-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lupus-nephritis-disparities-amongst-hospitalizations-in-the-united-states-a-national-inpatient-sample-study/