Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
Anti-Sm autoantibody has been a known specific biomarker of systemic lupus erythematosus (SLE). There have been reports about its correlation with higher disease activity, renal involvement, and lower lupus low disease activity state attainment (LLDAS) among SLE patients. However, its exact role in renal outcome among patients with known lupus nephritis (LN) has been uncertain. This study adds to the literature in the role of Anti-Sm in relation to its prognostic value among patients with lupus nephritis. We also investigate the effect of LLDAS among patients with anti-Sm.
Methods:
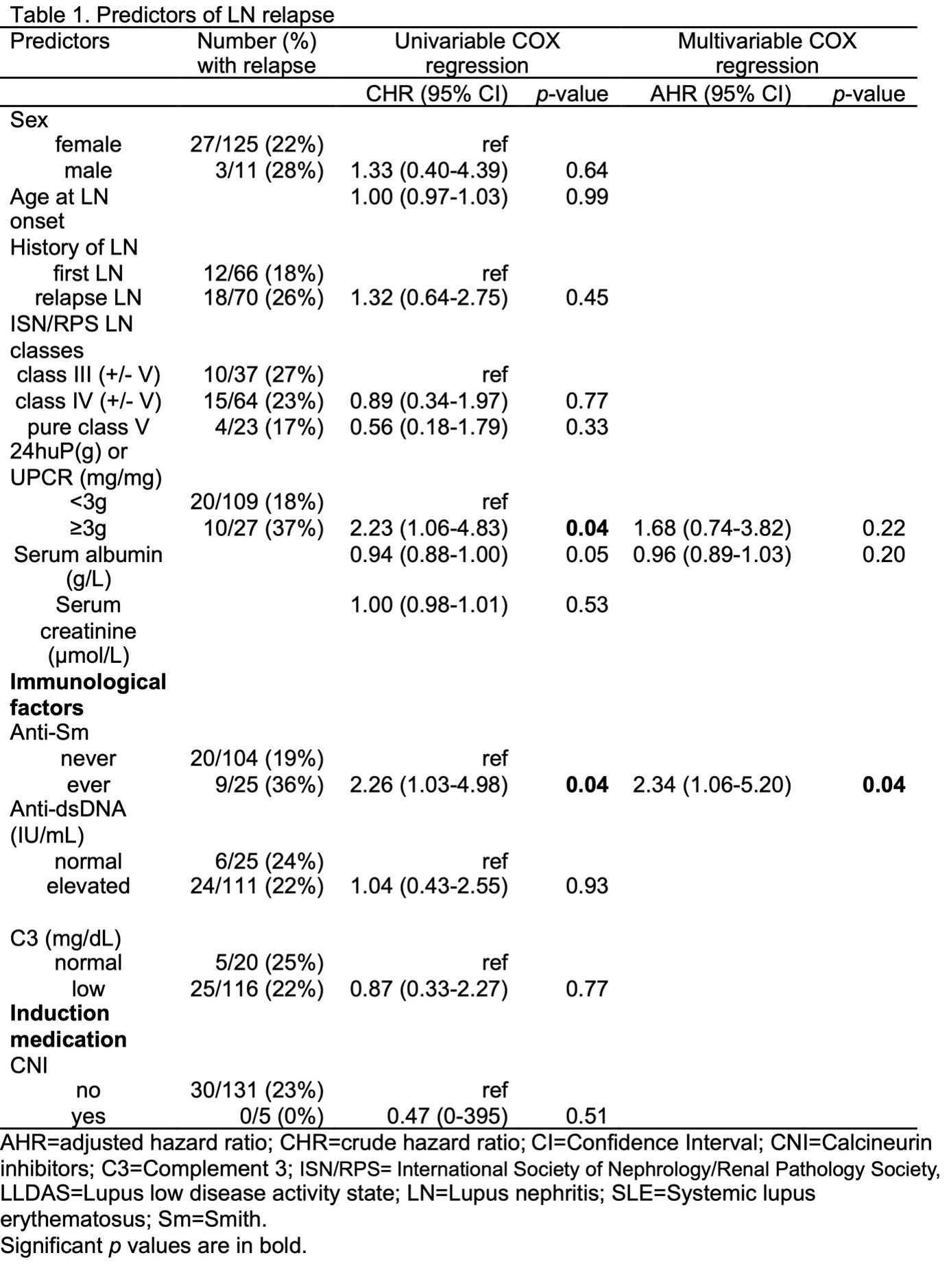
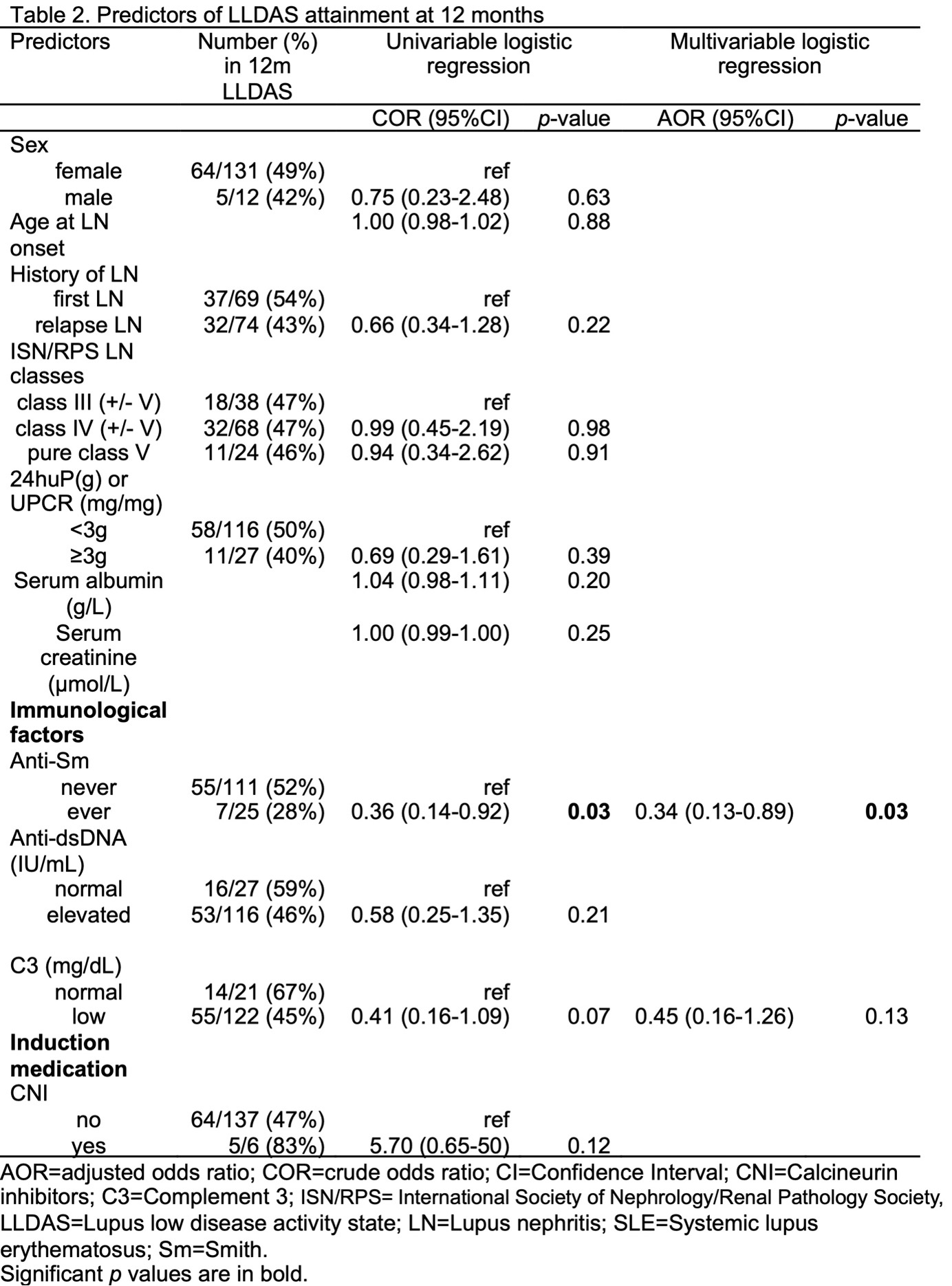
Patients with biopsy-proven LN during 2010-2020 were included. Baseline demographics, blood parameters and urinalysis results were recorded. Immunological markers such as autoantibodies profile were also documented. Complete or partial renal response (CRR/PRR) and LLDAS was assessed at 12 months post-LN, and any future relapses were recorded. LLDAS was attained by meeting: (1) SLE Disease Activity Index ≤4 with no major organ activity; (2) no new lupus disease; (3) physician global assessment ≤1; (4) prednisolone dose ≤7.5mg; (5) standard maintenance immunosuppressants. Relapse was a biopsy-proven LN after an initial treatment response of proteinuria reduction of ≥50% to sub-nephrotic range. Predictors of LLDAS and relapse were tested by logistic regression and COX regression respectively.
Results: A total 143 patients were included in this study. Anti-Sm positivity was present in 25 patients. Nephrotic range proteinuria and the presence of anti-Sm autoantibody were significant predictors of relapse in the univariable COX model. Only anti-Sm autoantibody was significant (p = 0.04) at the multivariable analysis. Anti-Sm autoantibody was the only variable found to predict LLDAS attainment (p = 0.03). Patients with anti-Sm had lower chance of LLDAS attainment (odds ratio = 0.34) with higher risk of subsequent relapse (hazard ratio = 2.34) compared to anti-Sm negative patients. Despite this, LLDAS attainment complementary to CRR/PRR was still found to be protective from future relapse (p < 0.001).
Conclusion:
Patients with anti-Sm belonged to a high-risk subgroup with worse prognosis, yet LLDAS attainment could still prevent subsequent relapse among them.
To cite this abstract in AMA style:
Cheung C, Lau C, Chan S. Lupus Low Disease Activity State Ameliorates the Poor Prognosis in Lupus Nephritis Patients with anti-Sm Autoantibody [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/lupus-low-disease-activity-state-ameliorates-the-poor-prognosis-in-lupus-nephritis-patients-with-anti-sm-autoantibody/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lupus-low-disease-activity-state-ameliorates-the-poor-prognosis-in-lupus-nephritis-patients-with-anti-sm-autoantibody/