Session Information
Session Type: Poster Session B
Session Time: 9:00AM-10:30AM
Background/Purpose: Cutaneous lupus erythematosus (CLE) is a manifestation of systemic lupus erythematosus (SLE) that can cause significant patient distress and disfiguration secondary to scar. Scarring mechanisms remain poorly understood and interventions for preventing or treating scarring are lacking in SLE/CLE. Fibroblasts (FBs) are involved in the regulation of immune responses, inflammation, and scarring, yet the role of inflammatory mediators on FB function in SLE is unclear. Here, we examined the inflammatory phenotype in FBs isolated from non-lesional skin from healthy controls (HC), and SLE patients with and without scarring CLE.
Methods: Non-lesional punch biopsies were obtained from University of Michigan patients with SLE (n=21), divided into patients with scarring skin lesions (n=8) and non-scarring skin lesions (n=13), as well as HCs (n=34). Scarring disease status was determined using the damage score of the Cutaneous Lupus Erythematosus Disease Area and Severity Index (CLASI). FBs were isolated from punch biopsies, cultured, and stimulated with IFN-γ, IFN-ɑ, TNF-ɑ, TGF-????, IL-1????, or UV light. RNA sequencing was performed and differentially expressed genes (DEGs) were determined using DESeq2 with log2FC > 0.6 and adjusted p-value < 0.05. Pathway analysis was performed by filtering the genes with the largest effect size (log2FCCLE – log2FCHC) to identify pathways shared across all stimulations and unique to individual stimulations.
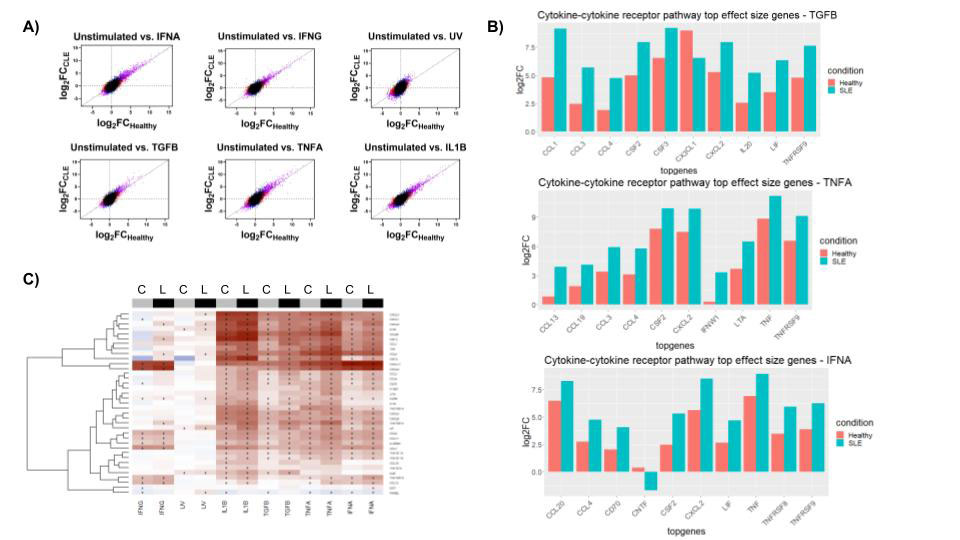
Results: HC and SLE FBs exhibited differential gene expression following cytokine treatment, with the largest effect size differences for TGF-????, TNF-ɑ, IFN-γ, and IFN-ɑ stimulation. Cytokine-cytokine receptor signaling pathway genes were upregulated across all conditions, with relatively more upregulation in SLE FBs in comparison to healthy controls. DEGs included CXCL and CCL genes, interleukins, and TNF. (Fig 1)
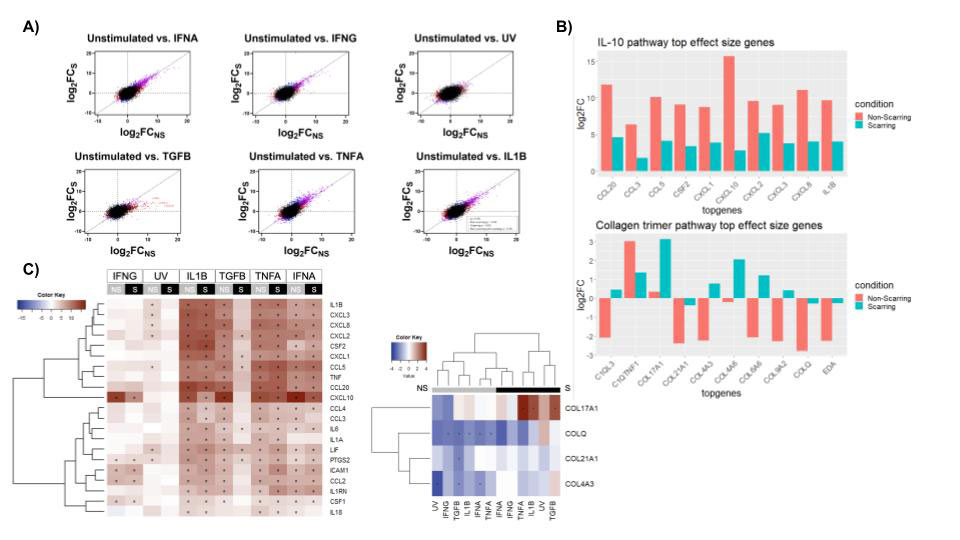
Pathway analysis of the scarring and non-scarring states revealed DEGs in the IL-10 pathway, especially specific to stimulation with TGF-????, a known fibrotic factor involved in myofibroblast activation. Interestingly, non-scarring patients had greater upregulation of proinflammatory signatures, including CXCL and CCL genes, and interleukins. Collagen trimer pathway genes were also significantly differentially expressed between scarring and non-scarring states. COL17A1 was up-regulated in scarring, especially after inflammatory signals like TGF-????, TNF-ɑ, and IL-1????, while COLQ, COL21A1, and COL4A3 were generally down-regulated in non-scarring. Histologic confirmation of collagen staining identified pro-fibrotic collagen expression in scarring skin lesions, near inflammatory infiltrates. (Fig 2)
Conclusion: Our results show that while exposure to inflammatory cytokines successfully up-regulates inflammatory pathways in both healthy and SLE fibroblasts, the effect is magnified in SLE. Furthermore, while all SLE fibroblasts are associated with elevated inflammation, FBs from patients who scar associated with upregulation of collagen pathways after TGF-β stimulation. Together, these findings provide important insights into the mechanisms of scarring in CLE and potential targets for intervention.
To cite this abstract in AMA style:
Shoffner-Beck S, Abernathy-Close L, Lazar S, Hurst A, Dobry C, Pandian D, Wasikowski R, Arnold K, Gudjonsson J, Tsoi L, Kahlenberg J. Lupus Fibroblasts from Non-lesional Skin Exhibit Exaggerated Responses to Inflammatory Cytokines and Upregulate Pro-fibrotic Collagens in Patients with Scarring Lesions [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/lupus-fibroblasts-from-non-lesional-skin-exhibit-exaggerated-responses-to-inflammatory-cytokines-and-upregulate-pro-fibrotic-collagens-in-patients-with-scarring-lesions/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lupus-fibroblasts-from-non-lesional-skin-exhibit-exaggerated-responses-to-inflammatory-cytokines-and-upregulate-pro-fibrotic-collagens-in-patients-with-scarring-lesions/