Session Information
Date: Sunday, November 13, 2022
Title: Vasculitis – Non-ANCA-Associated and Related Disorders Poster II
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic (VEXAS) syndrome is a recently identified disorder caused by somatic mutations in the UBA1 gene of myeloid cells. Pulmonary involvement has been reported, but a detailed description of lung involvement and radiologic findings is lacking.
Methods: A retrospective cohort study was conducted of all patients identified at the Mayo Clinic with VEXAS syndrome since October 2020. Clinical records and chest high resolution computed tomography (HRCT) scans were reviewed.
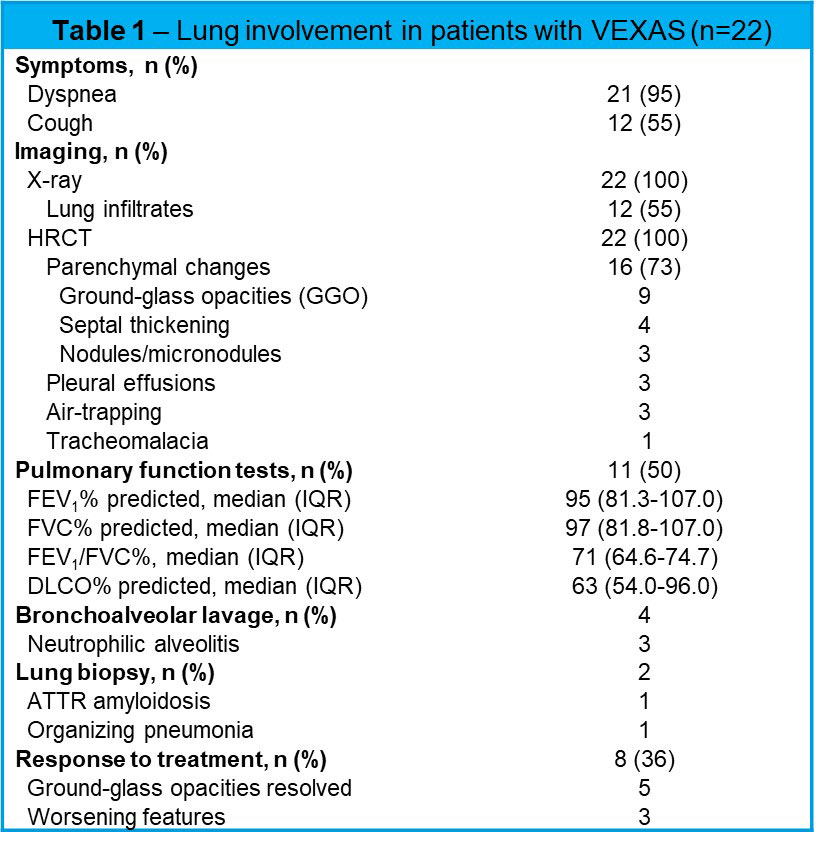
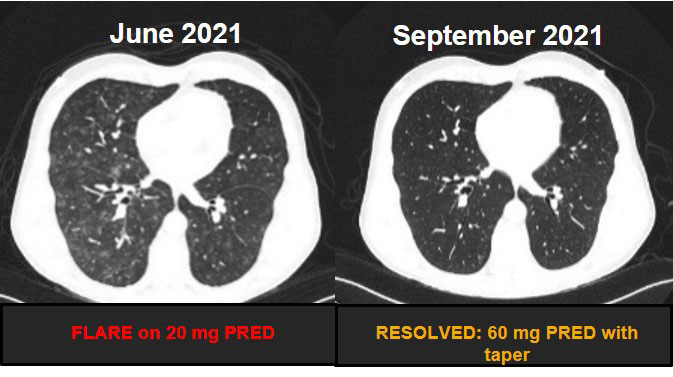
Results: Our cohort comprised 22 white men with a median age of 69 years (range 57-84). Hematologic disorders including multiple myeloma, myelodysplastic syndrome and pancytopenia were present in 10 patients (45%), rheumatologic diseases including granulomatosis with polyangiitis, IgG4-related disease, polyarteritis nodosa, relapsing polychondritis, and rheumatoid arthritis were found in 10 patients (45%), and 4 patients had dermatologic presentations including Sweet syndrome, Schnitzer-like syndrome or drug rash with eosinophilia skin syndrome (DRESS). VEXAS syndrome related features included fever (18,82%), skin lesions (20,91%), lung infiltrates (12,55%), chondritis (10,45%), venous thromboembolism (12,55%), macrocytic anemia (21,96%), and bone marrow vacuoles (22,100%). The somatic mutations affecting methionine-41 (p.Met41) in UBA1 gene were: 11 (50%) p.Met41Thr, 7 (32%) p.Met41Val, 2 (9%) p.Met41Leu, and 2 (9%) in the splice site. All patients received glucocorticoids (GC) (median duration of treatment was 2.6 years); 21 (96%) received conventional immunosuppressive agents (methotrexate, azathioprine, mycophenolate, leflunomide, cyclosporin, hydroxychloroquine, tofacitinib, ruxolitinib) and 9 (41%) received biologic agents (rituximab, tocilizumab, infliximab, etanercept, adalimumab, golimumab, abatacept). Respiratory symptoms included dyspnea and cough present in 21 (95%) and 12 (55%). Bronchoalveolar lavage (BAL) was available in 4 patients, with neutrophilic alveolitis in 3. Two patients had lung biopsies that showed ATTR amyloidosis and organizing pneumonia with lymphoid interstitial pneumonia, respectively. Pulmonary function tests were available in 9 (41%) patients and showed normal results in 5; 3 patients had isolated reduction in DLCO and 1 had mild restriction. On chest HRCT, 16 patients (73%) had parenchymal changes including ground-glass opacities in 9, septal thickening in 4, and nodules in 3; pleural effusions were present in 3 patients, air-trapping in 3 patients and tracheomalacia in 1 patient. Follow-up chest HRCT was available for 8 patients (36%), the ground-glass opacities resolved in 5 patients, 3 patients manifested new or increased ground-glass opacities, and 1 patient had increased interlobular septal thickening. VEXAS flares occurred in 18 patients (82%), the maximum number of relapses was 7, and they were mainly managed with GC and with changes in the immunosuppressive regimen.
Conclusion: Pulmonary involvement was documented by chest HRCT in most patients with VEXAS syndrome. The pulmonary manifestations of VEXAS are nonspecific and characterized predominantly by inflammatory parenchymal involvement.
To cite this abstract in AMA style:
Casal Moura M, Baqir M, Tandon Y, Samec M, Reichard K, Mangaonkar A, Go R, Warrington K, Patnaik M, Koster M, Ryu J. Lung Involvement in VEXAS Syndrome [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/lung-involvement-in-vexas-syndrome/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lung-involvement-in-vexas-syndrome/