Session Information
Date: Sunday, November 13, 2022
Title: Osteoporosis and Metabolic Bone Disease – Basic and Clinical Science Poster
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Inflammatory rheumatic and musculoskeletal diseases (iRMD) are associated with increased systemic bone loss that is mediated by chronic inflammation, treatment with glucocorticoids (GC), and other factors, leading to an increased risk of osteoporosis and fragility fractures. Our objective was to analyze the impact of variables that influence osteoporosis in patients with iRMD treated with GC.
Methods: Rh-GIOP is a prospective observational cohort study investigating bone health in consecutive patients with iRMD and current or prior GC treatment. We present an analysis of the patients’ baseline data here. Bone mineral density (BMD) measured by dual X-ray absorptiometry (DXA) was the primary outcome. Multivariable linear regression models were performed to identify variables associated with BMD. The focus lay on analyzing the impact of current GC dose on BMD as well as the impact of the interaction between GC dose and disease activity.
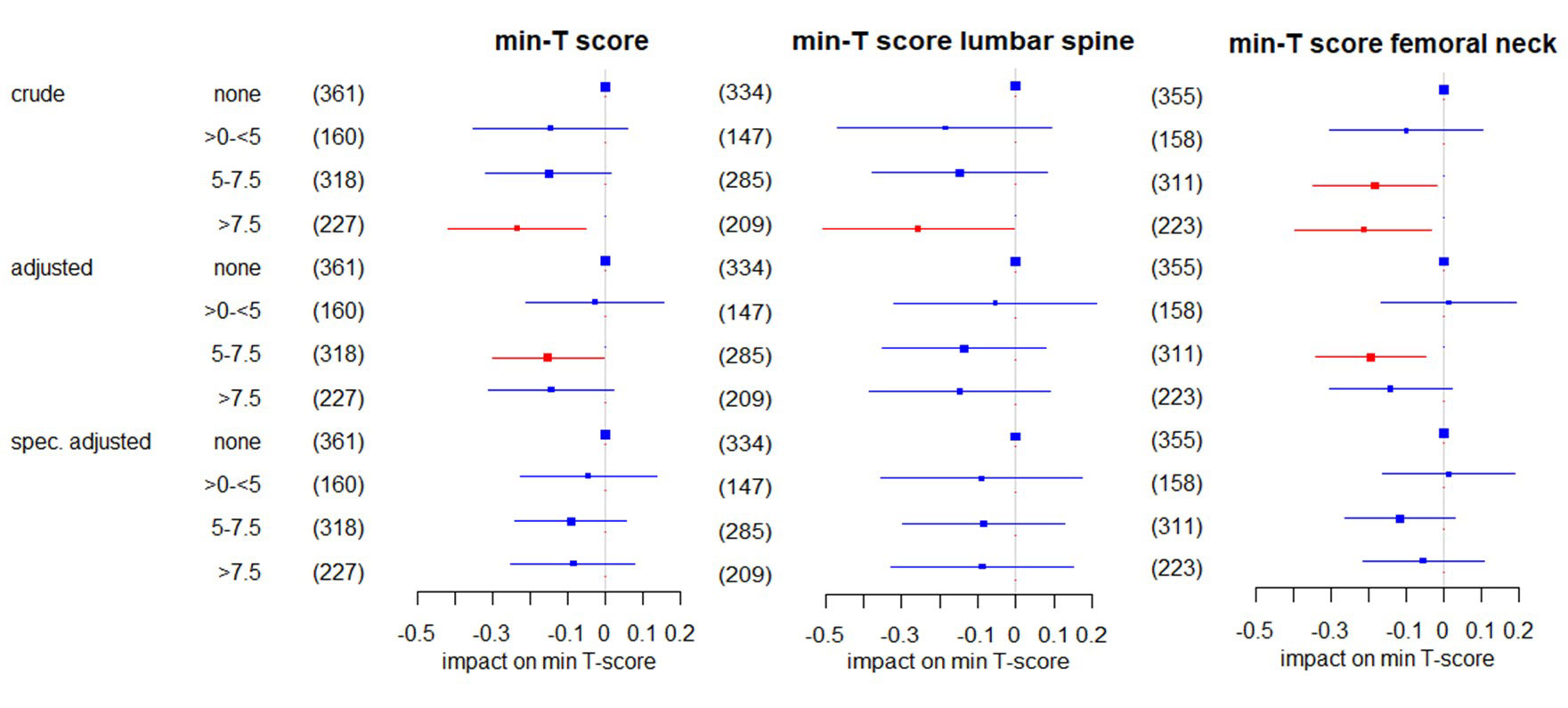
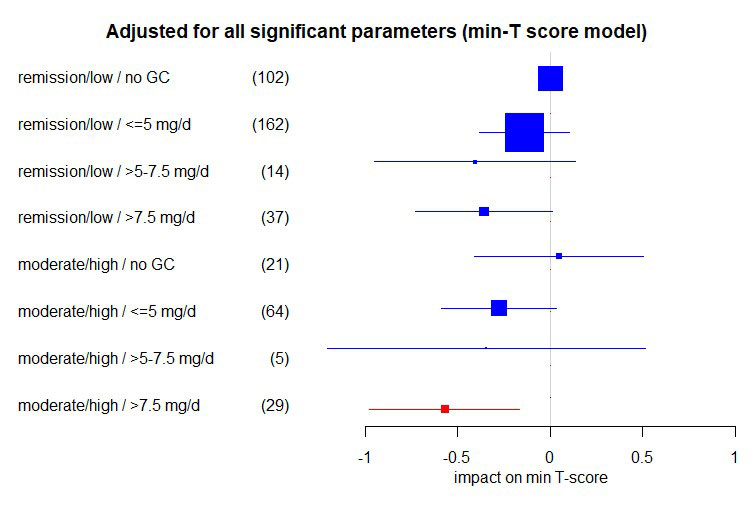
Results: Data from 1,066 patients with iRMD were analyzed. GC doses of < 5 mg prednisone equivalent per day, cumulative dose and duration of GC therapy were not associated with negative effects on BMD. Dosages ≥5 mg/d lost their negative association with BMD after adjustment for confounders. When sub-analyzing patients with exactly 5 mg/d, no negative effect was seen. For patients with rheumatoid arthritis (RA), GC doses >7.5 mg per day showed a negative association with BMD overall, but this effect seemed to be specific only to patients with moderate or high disease activity (DAS28-CRP >3.2).
Conclusion: Glucocorticoids ≤5 mg/d did not seem to be associated with a reduction of BMD in patients with iRMD and current or prior exposure to GC. This is most likely due to the dampening of inflammation by GC, which exerts a mitigating effect on the risk of osteoporosis. We conclude that in patients with iRMD a) both optimal disease control, optimum glucocorticoid doses and sufficient osteoporosis treatment measures (such as normal vitamin D levels, appropriate use of anti-osteoporosis drugs) are essential for bone protection, and b) low GC dosages (≤ 5 mg/d), aimed at achieving sustained remission or low disease activity, are likely to be safe in terms of bone health.
To cite this abstract in AMA style:
Wiebe E, Huscher D, Schaumburg D, Palmowski A, Hermann S, Buttgereit T, Biesen R, Burmester G, Palmowski Y, Boers M, Stone J, Dejaco C, Buttgereit F. Low-Dose Prednisolone (≤5 Mg/d) Is Not Associated with Deleterious Effects on Bone Mineral Density: Baseline Findings in a Cohort of Rheumatic Disease Patients with Prior Glucocorticoid Exposure [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/low-dose-prednisolone-%e2%89%a45-mg-d-is-not-associated-with-deleterious-effects-on-bone-mineral-density-baseline-findings-in-a-cohort-of-rheumatic-disease-patients-with-prior-glucocorticoid-exposu/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/low-dose-prednisolone-%e2%89%a45-mg-d-is-not-associated-with-deleterious-effects-on-bone-mineral-density-baseline-findings-in-a-cohort-of-rheumatic-disease-patients-with-prior-glucocorticoid-exposu/