Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with Systemic Lupus Erythematosus (SLE) are at an increased risk of infection owing to immunosuppressive therapy along with coexistent immune dysregulation. It is often difficult to differentiatebetween infection and disease activity in a patient with SLE who presents with fever. Though many markers have been studied, markers like procalcitonin, which has high specificity, are expensive and not available in resource poor countries. Thus, we planned to see if low cost markers can be useful to differentiate infection from disease flare in a patient of SLE with fever.
Methods: Patients with SLE (SLICC criteria) presenting with fever of more than 48 hours duration, from December 2018 to February 2020 were included in the study. Detailed history, clinical examination and investigations were done to assess for infection. In addition, neutrophil to lymphocyte ratio (N/L), neut-x, y, z indices1, Erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), C3, C4, anti-dsDNA antibodies and procalcitonin levels were measured. Neut-x and y indices are parameters obtained by objective evaluation of toxic granulation and the nuclear maturity of neutrophils by the Sysmex counter and Neut-z refers to the vector sum of the two.
Based on clinical assessment and laboratory data, fever episode was classified as infection, disease flare or both. The differences in variables between infection episode and disease flare were analyzed using Mann Whitney-U test for continuous and chi-square for categorical variables respectively, Binary logistic regression and ROC for multivariate analysis were used for analysis. In addition, a previously proposed low-cost calculator by Beca etal2was also validated and improved upon by addition of other variables.
Results: 42 episodes of fever were seen in 40 patients with SLE, and among these 18 were due to infection, 22 were related to disease activity and in 2 both infection and disease activity contributed to fever. The median age of the patients was 26.5 years with 90% being women. Two-thirds had a major organ involvement, distributed equally across the groups. Six patients with tuberculosis, viral and fungal infection were excluded from further analysis. High anti-dsDNA (p=0.002) and low complements(C3, p=0.02 and C4, p=0.0001) were characteristic of disease flare whereas high N/L ratio (p=0.04), high Neut-x (p=0.01), -y (p=0.04), -z (p=0.02), CRP (p=0.03), low ESR to CRP ratio (p=0.02) and high procalcitonin (p=0.0001) were seen with infection.
Using the 3 variables suggested by Beca etal i.e. days of fever, anti-dsDNA antibody and CRP the ROC curve had an area under curve (AUC) of 0.81 which increased to 0.91 when low complement levels, N/L ratio and Neut-z was added to this model. Replacing CRP with procalcitonin had higher AUC but it increased the cost.
Conclusion: A composite score oflow cost and routinely available parameters like days of fever, anti-dsDNA, low C3/C4, neutrophil to lymphocyte ratio and Neut-z gives a good discrimination between infection and flare in a febrile patient with SLE.
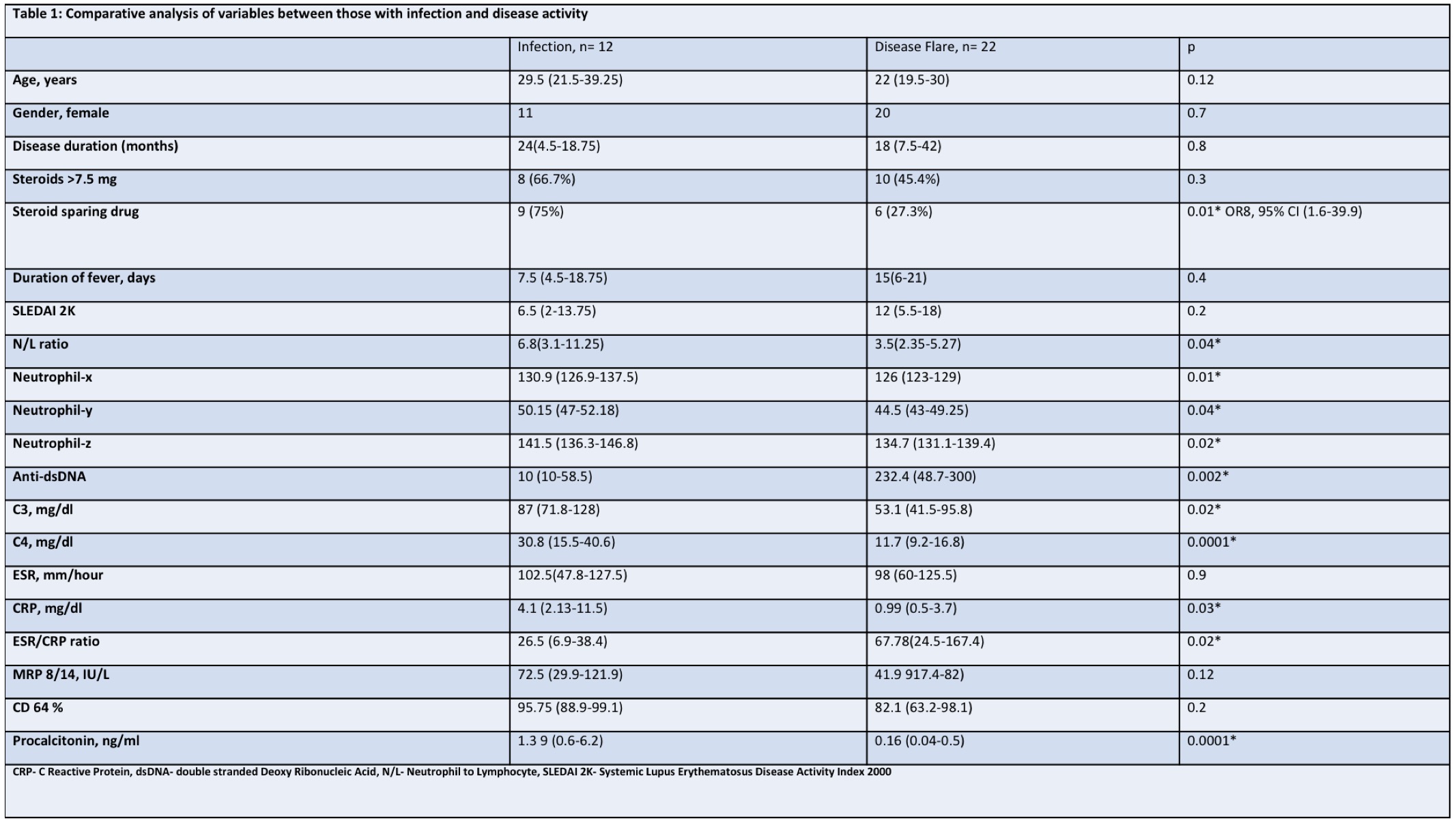 Table 1: Comparative analysis of variables between those with infection and disease activity
Table 1: Comparative analysis of variables between those with infection and disease activity
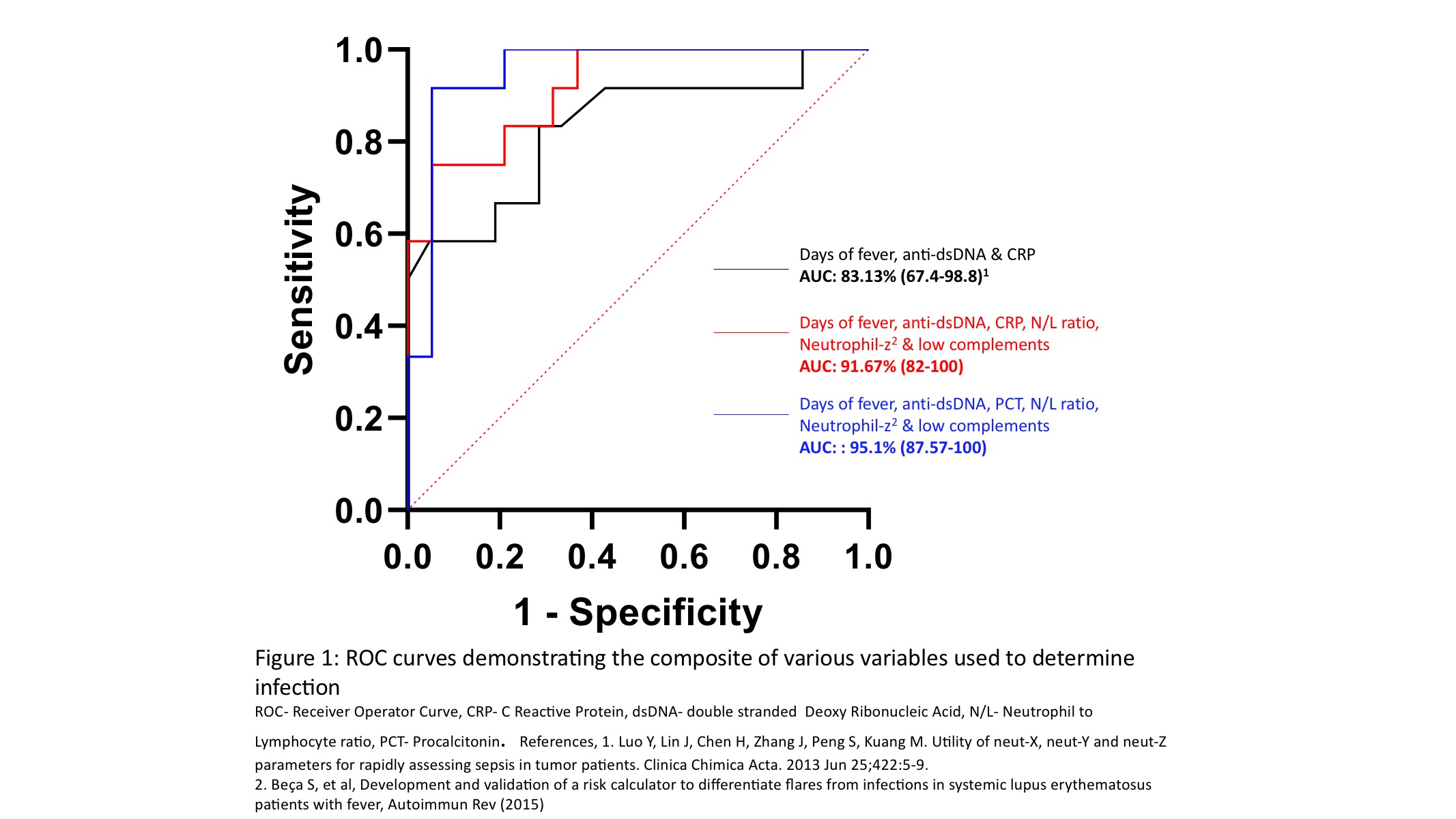 Figure 1: ROC curves demonstrating the composite of various variables used to determine infection
Figure 1: ROC curves demonstrating the composite of various variables used to determine infection
To cite this abstract in AMA style:
Mehta P, Singh K, Aggarwal A, Sharma S. Low Cost Composite Markers to Differentiate Infection from Disease Activity in a Febrile Patient with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/low-cost-composite-markers-to-differentiate-infection-from-disease-activity-in-a-febrile-patient-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/low-cost-composite-markers-to-differentiate-infection-from-disease-activity-in-a-febrile-patient-with-systemic-lupus-erythematosus/
