Session Information
Date: Sunday, October 21, 2018
Title: 3S089 ACR Abstract: Systemic Sclerosis & Rel D/O–Clinical I: Clinical Trials I (898–903)
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: The Scleroderma: Cyclophosphamide or Transplantation (SCOT) study established the long-term superiority of hematopoietic stem cell transplant (HSCT) over cyclophosphamide (CYC) [Sullivan KM, et al. N Engl J Med. 378:35-47]. The primary endpoint, a global rank composite score (GRCS) at 54 months, integrated multiple disease features, but is not a clinical score. Longitudinal trends in the GRCS components can identify changes in clinical progression. Because dropouts, death, or organ failure lead to early loss of subjects, analysis methods must account for data that are not “missing completely at random.”
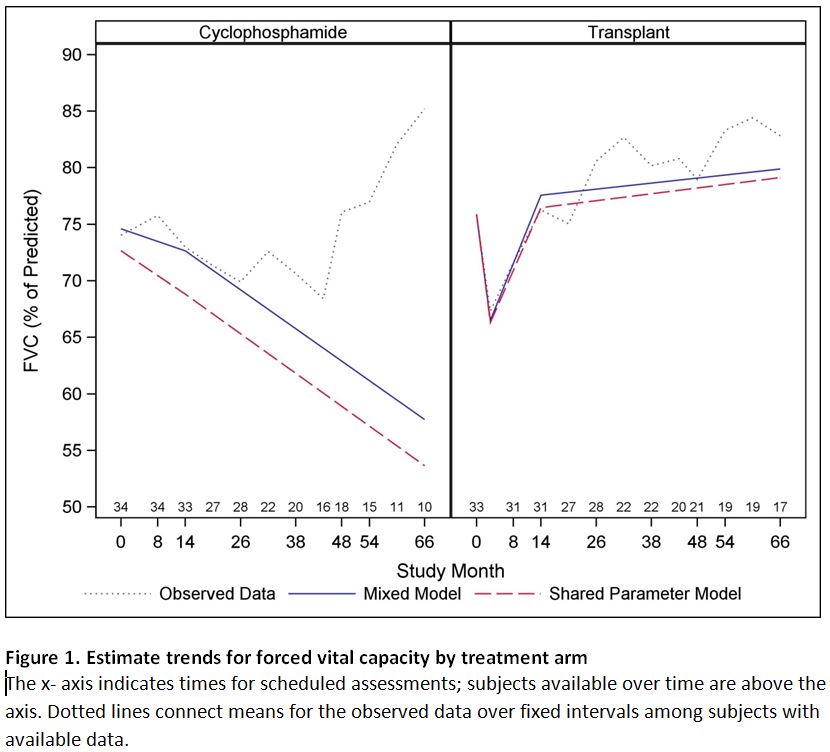
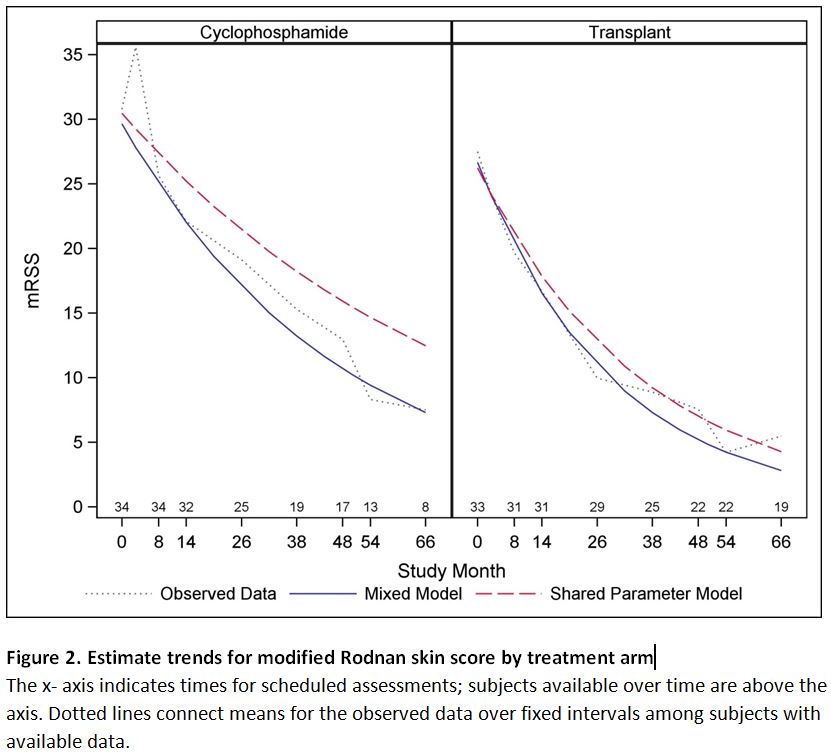
Methods: Data are from 33 HSCT recipients and 34 who completed ≥ 9 CYC doses. Diffusing capacity of carbon monoxide (DLCO), forced vital capacity (FVC), the Disability Index of the Health Assessment Questionnaire (HAQ-DI), and the modified Rodnan skin score (mRSS) were evaluated regularly up to month 72. For each, trends are compared using a mixed model (MX) that assumes data for subjects lost prematurely continue on their observed trajectories. Joint longitudinal/survival shared-parameter (SP) models that assume missingness is not “ignorable” are used for sensitivity. Figures display trends for observed means and model based fixed effects.
Results: In both arms, observed means for FVC increase over time; as those with poor FVCs are lost, the means for “survivors” go up (Figure1, dotted line). After accounting for subject loss, trends differ between the treatments. For HSCT, after an expected initial fall, the mean increase per year after month 14 was 0.53 percentage points compared to -3.44 for CYC (p=0.005, MX). Trends for MX and SP models are similar for HSCT, but the SP model suggests an even greater fall for CYC.
mRSS declined exponentially over time in both arms. The yearly decay rate was 0.41 for HSCT and 0.26 for CYC (p=0.05,MX). In both arms, MX and observed trends track closely suggesting that trajectories are similar for those lost early and those completing follow up. Trends for SP models are similar with slower decays rates. (Figure 2)
DLCO and HAQ-DI trends are summarized in Table 1.
Conclusion: Failure to account for early loss of longitudinal data may distort estimates of trends over time. Using two models, these analyses demonstrate the clinical superiority of HSCT over CYC for all components of GRCS even though mRSS improved in both arms.
To cite this abstract in AMA style:
Keyes-Elstein L, Goldmuntz E, Pinckney A, Crofford L, Furst DE, Mayes MD, McSweeney P, Nash R, Welch B, Sullivan K. Longitudinal Trends in Clinical Disease Features after Myeloablative Autologous Stem-Cell Transplantation or Cyclophosphamide in Severe Scleroderma [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/longitudinal-trends-in-clinical-disease-features-after-myeloablative-autologous-stem-cell-transplantation-or-cyclophosphamide-in-severe-scleroderma/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/longitudinal-trends-in-clinical-disease-features-after-myeloablative-autologous-stem-cell-transplantation-or-cyclophosphamide-in-severe-scleroderma/