Session Information
Session Type: Abstract Session
Session Time: 3:00PM-4:00PM
Background/Purpose: Central pain sensitization is a major contributor to pain severity in knee osteoarthritis (OA). Central sensitization is induced by neuroplastic changes in the central nervous system, which may potentially occur in response to peripheral input from OA, but may also be present in individuals unrelated to OA (i.e., an inherent trait). Neuroplastic changes are likely affected by numerous biological and sociocultural factors that vary within and between individuals over time. Therefore, patterns in central sensitization over time may also vary and influence pain severity differently. We sought to agnostically identify central sensitization trajectory patterns over nine years and evaluate their associations with pain severity in people with or at risk of knee OA.
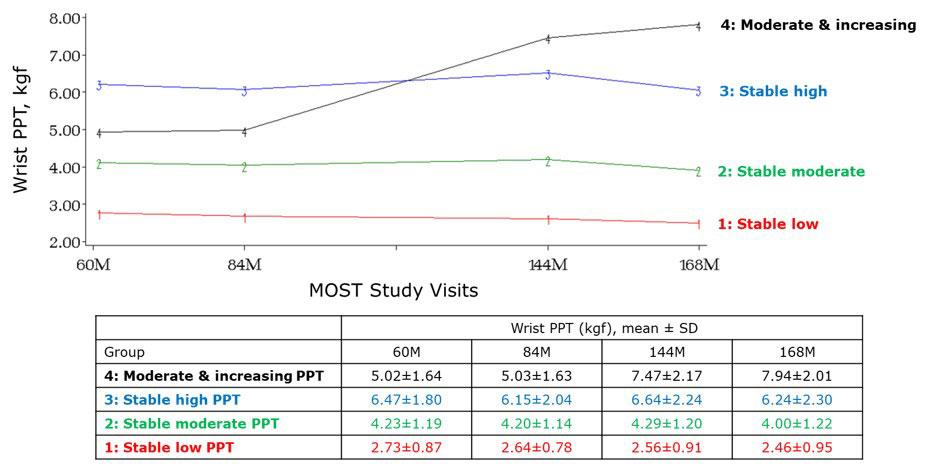
Methods: We included participants from the Multicenter Osteoarthritis (MOST) Study, a NIH-funded longitudinal cohort study of persons with or at risk of knee OA. We used data from 60- (the first visit at which central pain sensitization was assessed), 84-, 144-, and 168-month study visits. We assessed central pain sensitivity using pressure pain threshold (PPT) at the wrist, with a lower value reflecting a greater pain sensitivity. We agnostically identified wrist PPT trajectory groups over the nine years, using a discrete mixture model clustering. We evaluated the goodness of fit between individuals and corresponding trajectory groups by assessing the posterior probability of group membership. We evaluated the relation of wrist PPT trajectory groups to mean WOMAC pain of both knees at 168-months using linear regression, adjusting for age, sex, BMI, race, depressive symptom, and catastrophizing.
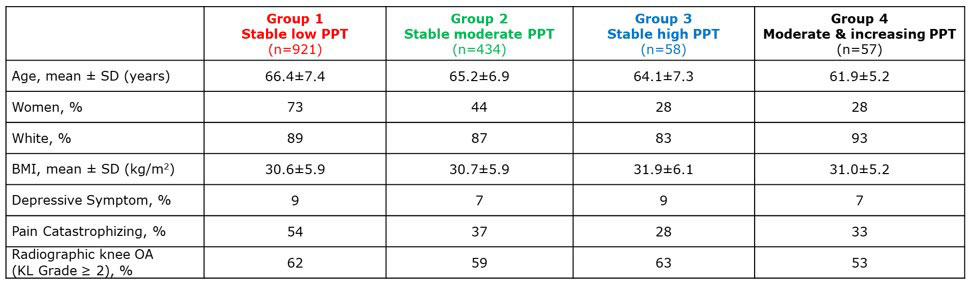
Results: We included 1470 participants (mean age 65.8±7.2, 60% female, mean BMI 30.0±5.9). Four distinct trajectory groups were identified: group 1 [stable low PPT, n=921 (62.3%)], 2 [stable moderate PPT, n=434 (29.5%)], 3 [stable high PPT, n=58 (4.0%)], and 4 [moderate & increasing PPT, n=57 (3.9%)](Figure). Participants characteristics per group are provided in the Table. The median posterior probability of group membership for groups 1-4 were 0.96, 0.85, 0.94, 0.97 respectively. Compared with group 1 (stable low PPT – most sensitized), group 2, 3 and 4 had 0.91 (95%CI -1.3, -0.5), 0.91 (95%CI -1.8, 0.0), and 1.67 (95%CI -2.6, -0.7) lower (better) WOMAC pain score than group 1 at the 168-month visit.
Conclusion: We found distinct central sensitization trajectory patterns over 9 years, which were associated with different levels of pain severity. Stable low PPT over a long period of time (i.e., most pain sensitized) was associated with greatest pain severity. Interestingly, one group appeared to have improvements in PPT over time (becoming less pain sensitized), potentially reflecting central adaptability to nociceptive input. Our findings highlight that some patterns of PPT remain stable over time, suggesting a trait phenomenon, whereas it can change in others, suggesting a potentially responsive phenomenon. These findings provide novel insights into potential contributors to the evolution of pain patterns over time, and support the possibility of pain sensitization being a trait in some, while a changeable state in others.
To cite this abstract in AMA style:
Aoyagi K, Wang N, Frey-Law L, Lewis C, Nevitt M, Neogi T. Longitudinal Trajectories of Central Pain Sensitization in People with or at Risk of Knee Osteoarthritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/longitudinal-trajectories-of-central-pain-sensitization-in-people-with-or-at-risk-of-knee-osteoarthritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/longitudinal-trajectories-of-central-pain-sensitization-in-people-with-or-at-risk-of-knee-osteoarthritis/