Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Fibromyalgia (FM) is a common comorbidity in patients with systemic lupus erythematosus (SLE) and a major contributor to poor health related quality of life. Distinguishing between SLE disease activity and FM as the source of chronic pain is critical since it would inform disease management and as well prevent unwarranted labeling of FM in patients’ medical records. Accordingly, this study leveraged a multi-racial/multi-ethnic lupus cohort representing a spectrum of manifestations to longitudinally characterize chronic pain phenotypes, associations with disease activity measures and evaluate the role of electroencephalography (EEG) as a potential diagnostic tool in these patients.
Methods: SLE patients enrolled in the NYU lupus cohort were screened for FM during in-person rheumatology visits from 9/22-4/24 using the 2016 ACR FM classification criteria and re-screened at a subsequent visit at least three months after initial screening (n= 102 patients, median follow up = 7 months). Hybrid SELENA-SLEDAI scores and medications were recorded at each visit. A subset of patients underwent EEGs at the follow up visit.
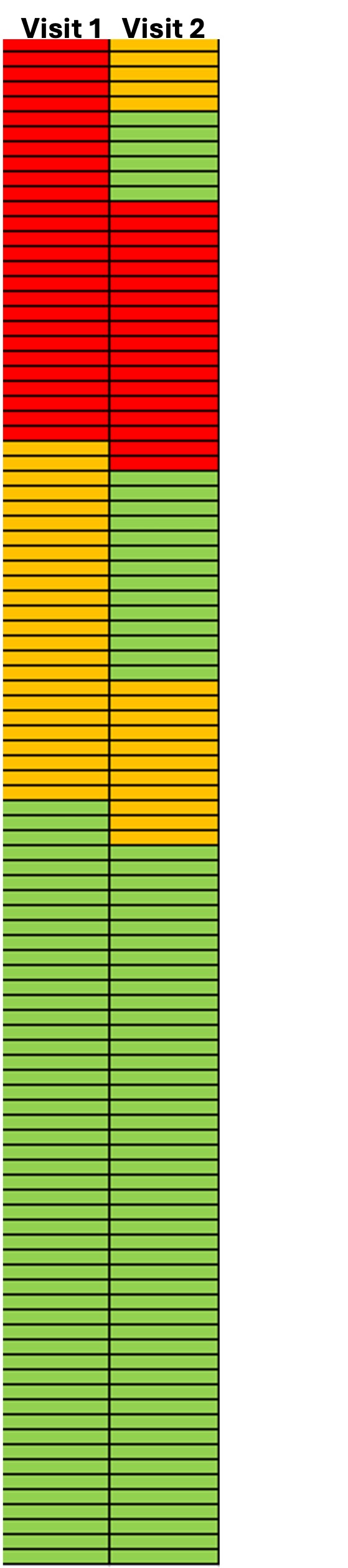
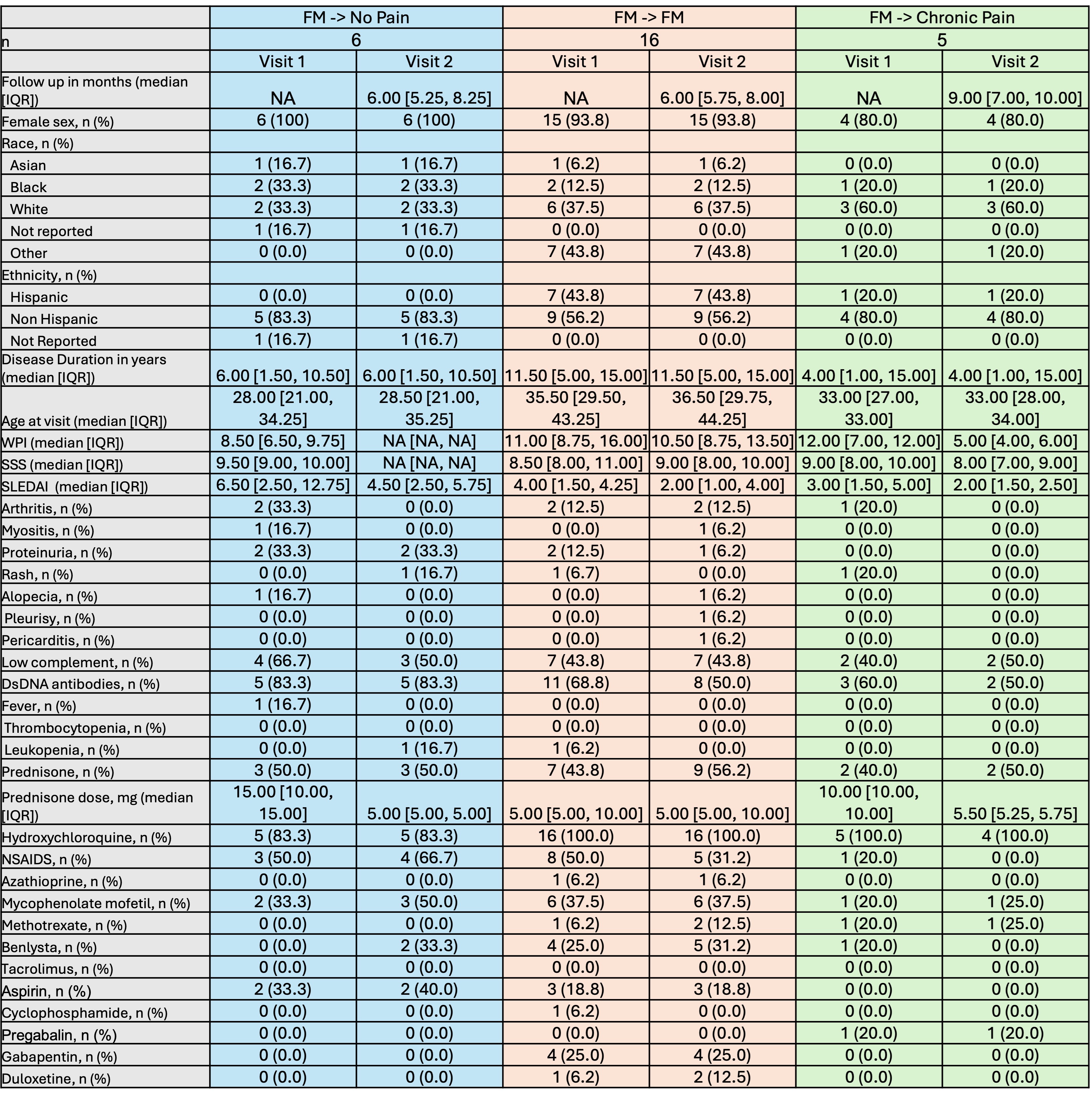
Results: At baseline, 51 (50%) patients had no chronic pain, 24 (24%) reported chronic pain without FM, and 27 (26%) patients met criteria for FM. Of the 51 patients without chronic pain, only 3 (6%) developed chronic pain and none had FM at subsequent visits (Figure 1). Of 24 patients reporting chronic pain without FM, 2 (8%) progressed to FM, 8 (33%) continued to report chronic pain without meeting criteria for FM, and 14 (58%) reported resolution of chronic pain. Of 27 patients with FM, 11 (41%) no longer met FM criteria at subsequent screening (5 still reported chronic pain and 6 reported no chronic pain). Focusing on these 27 patients with FM at baseline, those who no longer reported chronic pain at visit two had higher baseline SLE disease activity including more arthritis, myositis, proteinuria, alopecia, and low complement compared to those who continued to report chronic pain with/without meeting criteria for FM despite similar medication use (Table 1). At re-screening disease activity generally decreased for all groups but those initial FM patients no longer reporting chronic pain had resolution of arthritis, myositis, and alopecia. To date, EEGs have been performed on 8 patients at visit two (5 patients without chronic pain at both visits, 1 who transitioned from chronic pain to FM, and 1 each who had chronic pain and FM at both visits). EEGs appear to indicate that chronic pain patients show increased response to noxious inputs in the somatosensory cortex, and decreased response in the cingulate cortex, compared with patients with SLE without chronic pain. (Figure 2)
Conclusion: These data suggest that FM phenotypes in SLE patients are not stable over time and may be influenced by SLE disease activity. Even in patients with a high widespread pain index and symptom severity scale, clinicians should exercise caution before diagnosing FM in the presence of clinically active SLE unless symptoms persist despite decreases in disease activity. Preliminary EEG findings indicate altered cortical nociceptive processing in SLE patients with chronic pain.
To cite this abstract in AMA style:
Cohen B, Carlucci P, Corbitt K, Masson M, Saxena A, Belmont H, Tseng C, Wu R, Martinez H, Kenefati G, Doan L, Wang J, Barbour K, Gold H, Buyon J, Izmirly P. Longitudinal Patterns of Fibromyalgia Phenotypes in Patients with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/longitudinal-patterns-of-fibromyalgia-phenotypes-in-patients-with-systemic-lupus-erythematosus/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/longitudinal-patterns-of-fibromyalgia-phenotypes-in-patients-with-systemic-lupus-erythematosus/