Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
The aim of the study was to describe the evolution of mortality over recent decades in systemic necrotizing vasculitides, including polyarteritis nodosa (PAN), granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA).
Methods:
The date of diagnosis and the cause of death for patients with PAN, GPA, MPA, and EGPA were analyzed from the French Vasculitis Study Group database. Patients were divided into 5 groups: diagnosis before 1980, 1980-1989, 1990-1999, 2000-2010, and after 2010. The causes of death were classified as either vasculitis, infection, cardiovascular, malignancy, miscellaneous, or unknown.
Results:
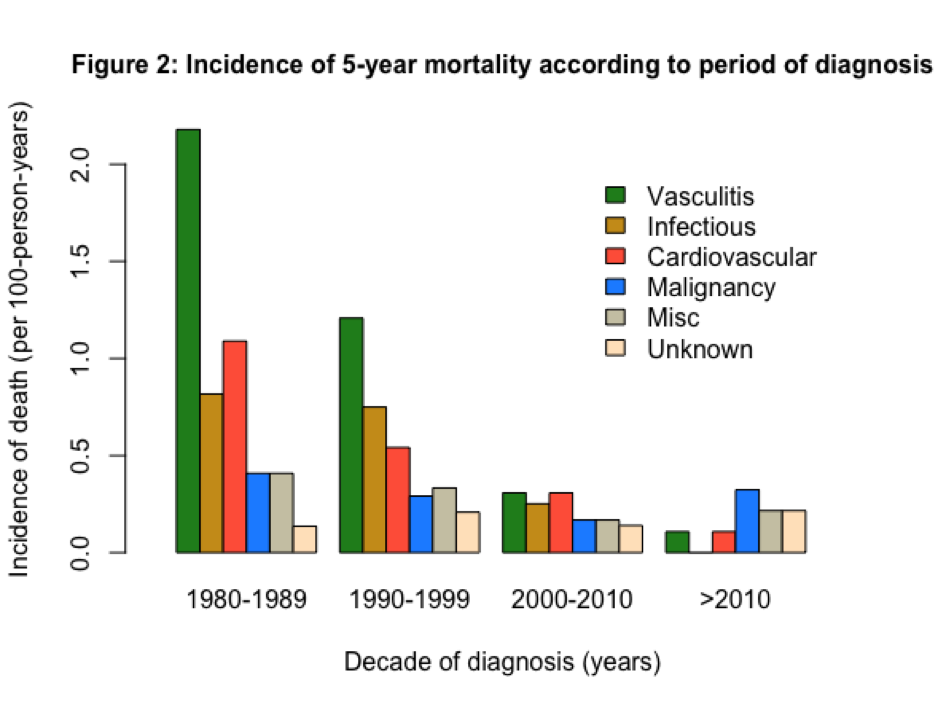
Among the 2243 included patients (PAN 16%, GPA 42%, EGPA 23%, MPA 19%), 301 (13%) deaths were reported (Table 1). The 5-year overall survival rate increased from 72.2% (95% confidence interval [CI] 59.7-87.2) for patients diagnosed before 1980, to 94.5% (95% CI 90.4-98.8) after 2010 (p<0.001; Figure 1). The incidence of 5-year mortality between 1980-1989 and the last decade (>2010) decreased from 2.18 to 0.11 per 100 person-years for vasculitis-related deaths (p=0.004), from 1.09 to 0.11 for cardiovascular-related deaths (p=0.03), and from 0.82 to 0.25 (p=0.03) for deaths caused by infection. No death by infection occurred in patients diagnosed after 2010. For deaths related to malignancy, the incidence of 5-year mortality was 0.41 per 100 person-years in 1980-1989, 0.17 in 2000-2009 (p=0.21), and 0.32 after 2010 (p=0.78).
Conclusion:
The results indicate that survival has dramatically improved since the 1980s due to the decrease of vasculitis flares and infections, but that cancer-related mortality remained stable. These results highlight the current targets to improve the overall prognosis.
|
Table 1 – Baseline characteristic of patients
|
|||||||
|
TOTAL
|
< 1980
|
1980-1989
|
1990-1999
|
2000-2009
|
³ 2010
|
p-value
|
|
|
Male sex ,% |
53.5 |
52.9 |
53.1 |
56.2 |
52.0 |
54.3 |
0.6 |
|
Mean age at diagnosis, years ± SD |
52.6 ± 16.8 |
38.6 ± 16.2 |
48.4 ± 16.3 |
51.2 ± 16.6 |
53.8 ± 16.6 |
55.6 ± 16.6 |
<0.001 |
|
Diagnosis, n (%)
|
|
||||||
|
PAN |
358 (16.0) |
28 (54.9) |
84 (42.8) |
118 (19.3) |
93 (9.4) |
35 (8.8) |
<0.001 |
|
GPA |
938 (41.8) |
0 (0) |
17 (8.7) |
245 (40.2) |
493 (50.0) |
183 (45.8) |
<0.001 |
|
EGPA |
511 (22.8) |
15 (29.4) |
64 (32.7) |
125 (20.5) |
212 (21.5) |
95 (23.8) |
0.004 |
|
MPA |
436 (19.4) |
8 (15.7) |
31 (15.8) |
122 (20.0) |
188 (19.1) |
87 (21.8) |
0.48 |
|
Mean duration of follow-up, years ± SD |
6.2 ± 5.8 |
9.6 ± 10.1 |
10.1 ± 9.1 |
8.2 ± 6.3 |
5.6 ± 4.0 |
2.4 ± 1.8 |
<0.001 |
|
Total number of deaths at 5 years
|
185
|
11
|
37
|
80
|
48
|
9
|
<0.001 |
|
Vasculitis
|
60
|
3
|
16
|
29
|
11
|
1
|
0.18 |
|
Infection
|
34
|
1
|
6
|
18
|
9
|
0
|
0.57 |
|
Cardiovascular
|
34
|
1
|
8
|
13
|
11
|
1
|
0.79 |
|
Malignancy
|
19
|
0
|
3
|
7
|
6
|
3
|
0.19 |
|
Miscellaneous
|
19
|
0
|
3
|
8
|
6
|
2
|
0.54 |
|
Unknown
|
19
|
6
|
1
|
5
|
5
|
2
|
<0.001 |
|
EGPA: eosinophilic granulomatosis with polyangiitis, GPA: granulomatosis with polyangiitis, MPA: microscopic polyangiitis, PAN: polyarteritis nodosa, SD: standard deviation. aPercentage calculated from the total number of patients. bPercentage calculated from the total number of deaths at 5 years in the same decade. |
|||||||
To cite this abstract in AMA style:
Jardel S, Puéchal X, Le Quellec A, Groh M, Hamidou M, Maurier F, Aumaître O, Aouba A, Quémeneur T, Subra JF, Cottin V, Godmer P, Cacoub P, Delaval P, Fauchais AL, Hachulla E, Maucort-Boulch D, Guillevin L, Lega JC. Long-Term Survival in Systemic Necrotizing Vasculitides [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/long-term-survival-in-systemic-necrotizing-vasculitides/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/long-term-survival-in-systemic-necrotizing-vasculitides/