Session Information
Date: Monday, November 11, 2019
Title: Pediatric Rheumatology – ePoster II: SLE, Juvenile Dermatomyositis, & Scleroderma
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Compared to adult-onset disease, pediatric-onset SLE (p-SLE) has more severe renal involvement. There are no population-based, long-term follow-up studies of pediatric lupus nephritis (LN) in the United States. This study characterized the long-term risk of end-stage renal disease (ESRD) in p-SLE.
Methods: The Georgia Lupus Registry is a population-based registry supported by the Centers for Disease Control and Prevention of validated SLE patients in 2 counties of Atlanta, Georgia. Trained abstractors reviewed medical records to validate incident SLE cases in 2002-2004 (baseline), including p-SLE (diagnosed < 18 years of age) using the following criteria: ≥ 4 ACR classification criteria for SLE or 3 criteria with a final diagnosis of SLE made by a board-certified rheumatologist. Patients were matched to the United States Renal Data System through 2015. ESRD cases were defined as being on dialysis or having received a renal transplant. Wilcoxon rank-sum tests were used to analyze continuous variables and Chi-squared (or Fisher’s exact) tests for categorical variables using SAS.
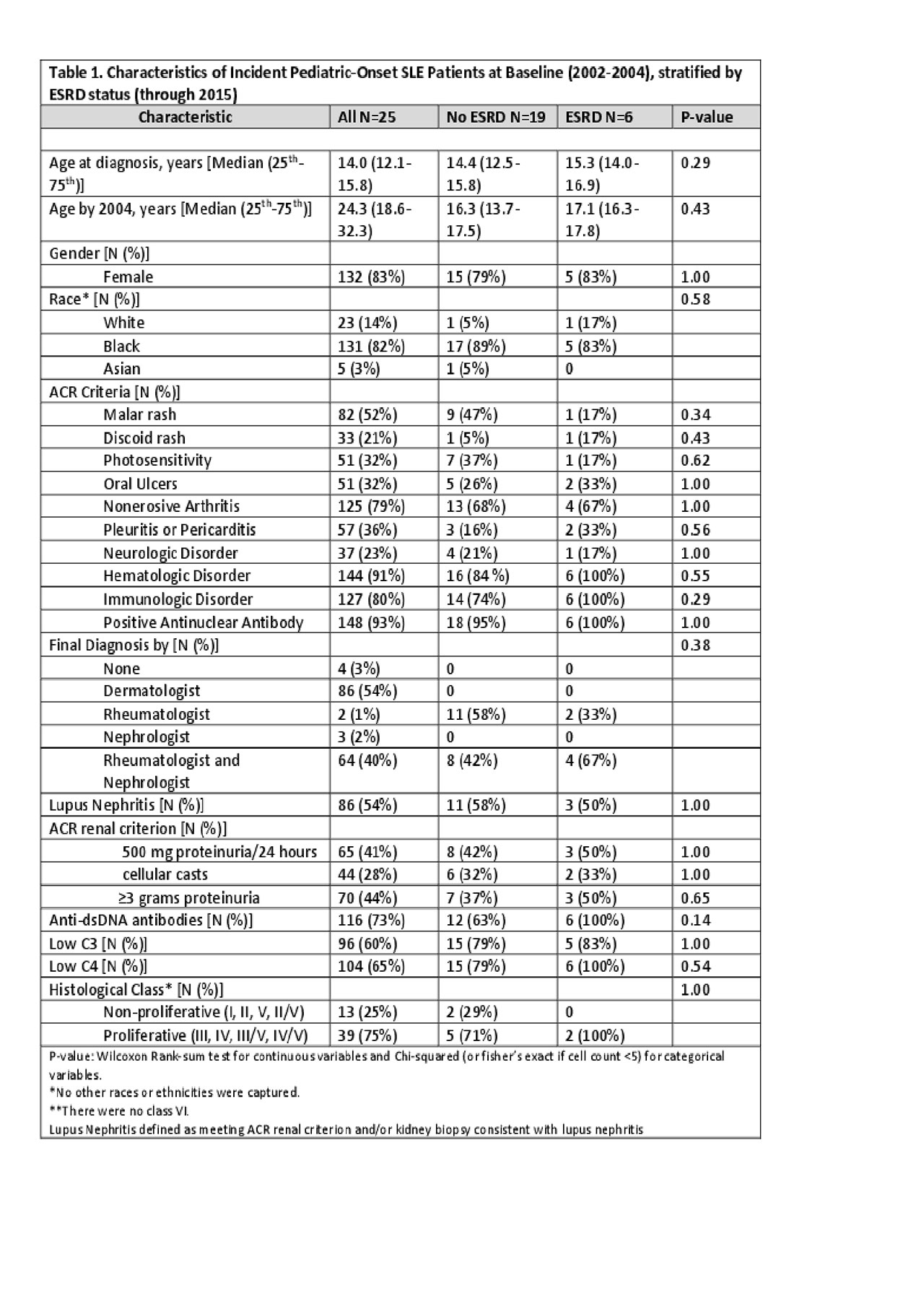
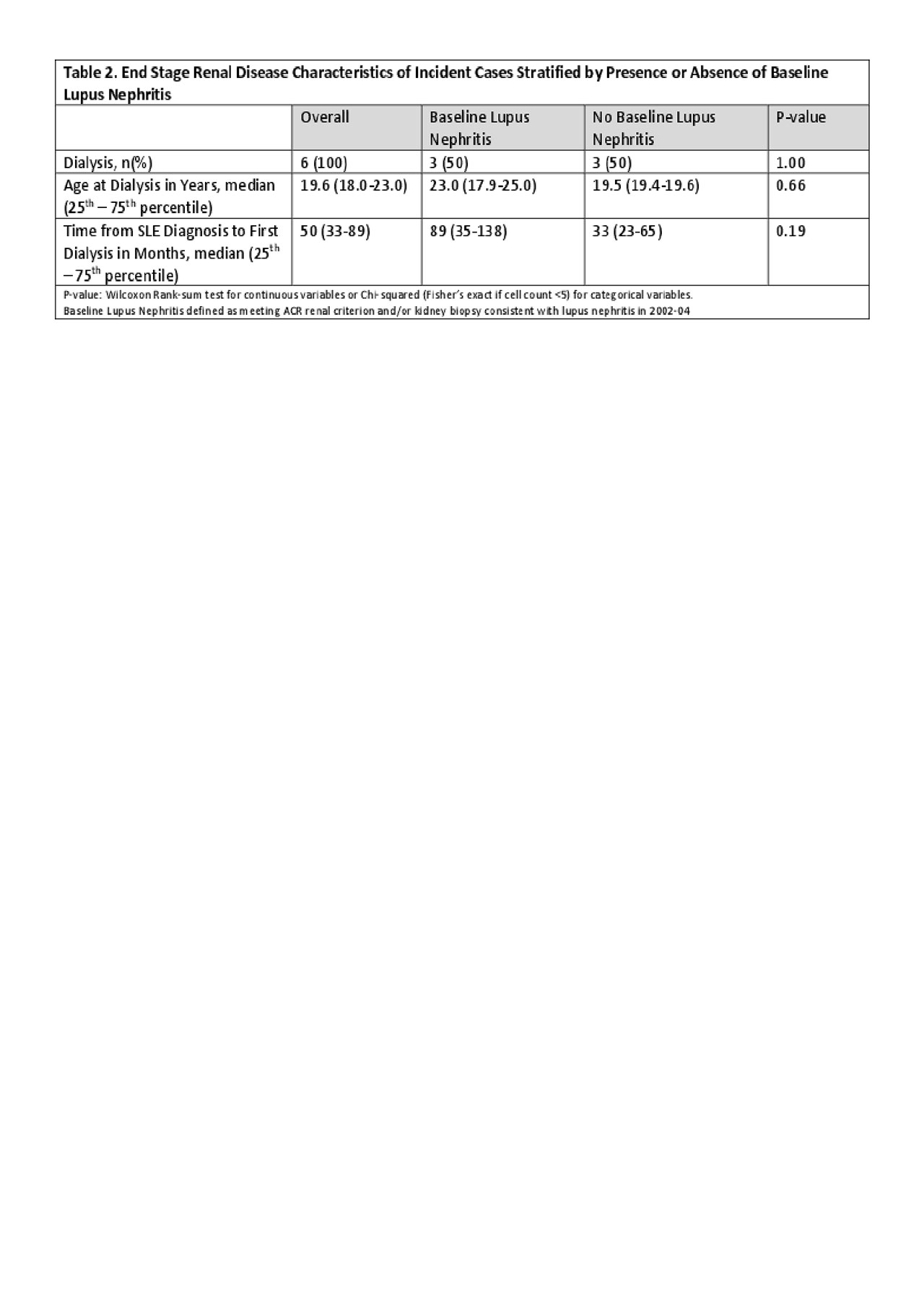
Results: The median age at diagnosis was 14 years (12.1–15.8), 82% were females, and 82% were black. Out of 25 incident cases, 6 (24%) developed ESRD through 2015. There were 14 (56%) who had LN at baseline, from which 3 (21.4%) developed ESRD. The other 3 ESRD cases had no record of renal involvement at baseline. There were no significant differences in baseline ACR criterion between those with and without eventual ESRD, including renal and immunologic parameters. Biopsy findings were not associated with ESRD (Table 1). The median age at first dialysis was 19.6 years, and the median time from SLE diagnosis to dialysis initiation was 50 months. Median age of dialysis initiation was 19.6 years. Those with baseline nephritis were slightly older (23.0 vs. 19.5 years, median) and had much longer time from SLE diagnosis to first dialysis (89 vs. 33 months, median) (Table 2).
Conclusion: This is the first population-based, long-term follow-up of validated p-SLE patients and their renal survival in an incident cohort. More than half had LN at baseline, with most maintaining renal survival during follow-up. However, after 12-14 years of follow-up, nearly a quarter of all p-SLE patients developed ESRD, and there were no associations between baseline clinical or immunologic characteristics and eventual ESRD. Various factors associated with p-SLE and the transition to adult care must be explored to improve long-term outcomes.
To cite this abstract in AMA style:
Park C, Figueroa J, Drenkard C, Plantinga L, Greenbaum L, Lim S. Long-term Renal Survival of Pediatric Onset Lupus Patients in a Population-Based Cohort [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/long-term-renal-survival-of-pediatric-onset-lupus-patients-in-a-population-based-cohort/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/long-term-renal-survival-of-pediatric-onset-lupus-patients-in-a-population-based-cohort/