Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Long-term Outcome of Pulmonary Sarcoidosis: A Population-Based Cohort Study from 1976-2013
Background/Purpose: A hallmark of sarcoidosis is lung disease, which has variable expression. This study was undertaken to better understand the course of pulmonary sarcoidosis.
Methods: A cohort of 311 incident cases of pulmonary sarcoidosis in a geographically well-defined population from 1976-2013 was identified from the comprehensive medical record-linkage system. Diagnosis of sarcoidosis required physician diagnosis supported by biopsy showing non-caseating granuloma, radiographic evidence of intrathoracic sarcoidosis and compatible clinical presentations without evidence of other granulomatous diseases. Medical records of the confirmed cases were reviewed from diagnosis to last follow-up. Data on stage of pulmonary sarcoidosis at diagnosis, serial pulmonary function tests (total lung capacity [TLC], force vital capacity [FVC], forced expiratory volume in 1 second [FEV1] and diffusing capacity for carbon monoxide [DLCO]), requirement of oxygen therapy and treatment were abstracted. The cumulative incidence of chronic respiratory impairment (defined as FVC of <50%, DLCO of <40% or requirement to use oxygen supplementation) adjusted for the competing risk of death was estimated. Cox models were used to assess the association of stage of pulmonary sarcoidosis and treatment on the development of chronic respiratory impairment.
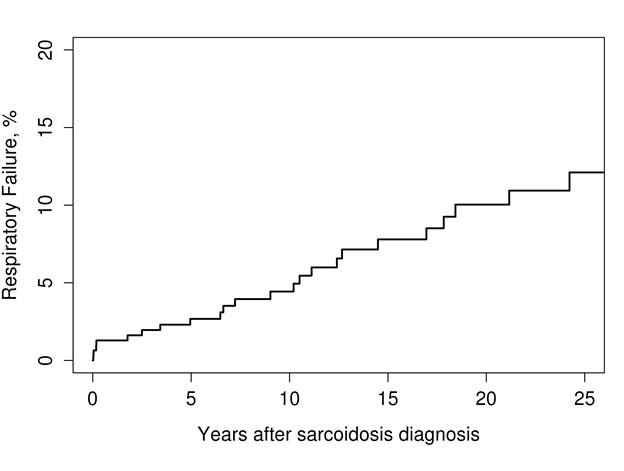
Results: The means of PFT measures at baseline in this cohort were 97.1%, 95.3%, 91.4% and 91.1% of predicted values for TLC, FVC, FEV1 and DLCO, respectively. At 5 years, the mean percentage predicted for TLC, FVC, FEV1 and DLCO declined by 1.6%, 3.5%, 4.3% and 3.1%, respectively. A total of 25 patients developed chronic respiratory impairment which corresponded to 10 year event rate of 4.4% (95% confidence interval [CI], 1.9%–6.9%) as demonstrated in figure 1. Stage of pulmonary sarcoidosis at diagnosis was a strong predictor for chronic respiratory impairment with hazard ratio (HR) compared with stage I of 5.29 (95% CI, 1.65–16.96) for stage II and 8.36 (95% CI, 26.3–26.52) for stage III and IV. Use of glucocorticoids and immunosuppressive agents was associated with a significantly increased risk of chronic respiratory impairment (HR 4.60; 95% CI, 1.94–10.88 and HR 5.13; 95% CI, 1.47–17.86, respectively). However, it is unlikely that treatment with glucocorticoids/ immunosuppressive agents had a deteriorative effect on pulmonary function. It is more likely that use of these medications is simply an indicator of more severe disease.
Conclusion: Patients with pulmonary sarcoidosis have a good pulmonary prognosis with a low incidence of chronic respiratory impairment.
Figure 1: Cumulative incidence of chronic respiratory impairment among 311 patients with pulmonary sarcoidosis
To cite this abstract in AMA style:
Ungprasert P, Crowson CS, Carmona Porquera EM, Matteson EL. Long-Term Outcome of Pulmonary Sarcoidosis: A Population-Based Cohort Study from 1976-2013 [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/long-term-outcome-of-pulmonary-sarcoidosis-a-population-based-cohort-study-from-1976-2013/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/long-term-outcome-of-pulmonary-sarcoidosis-a-population-based-cohort-study-from-1976-2013/