Session Information
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Hydralazine associated vasculitis (HAV) is rare but with potentially detrimental complications, affecting different organ systems. Most case series described short term disease course. Hence, data is sparse regarding long term management and outcome of HAV. The aim of this study is to determine long term outcome and whether variable duration of therapy has any impact on outcome.
Methods: We identified cases of HAV by searching electronic medical records for ICD codes of vasculitis and association of hydralazine intake from July of 2001 to July of 2017. Patients who received hydralazine after vasculitis onset were excluded. 23 patients were identified with diagnosis of HAV as deemed by the treating clinician. Data collected included demographics, hydralazine dose/duration, comorbid conditions, clinical presentation, laboratory, radiologic and pathological data, treatment strategies and outcomes. Continuous variables were summarized using means or medians, and categorical variables were summarized using frequencies and percentages. Outcomes were defined by full renal recovery, chronic kidney damage or relapse. Lung involvement was also registered.
Results: 23 patients (age 65.8±10.5 years, 65% males) with HAV were identified. Median duration of hydralazine use at onset of vasculitis was 34 months (5,170), with median total daily dose of 150 mg. Table 1 represents organ involvement, serological findings and treatment. The most commonly involved organs were the kidneys (100%) and lungs (48%). Majority of patients had positive serology (ANCA 100%, ANA 91%, anti-histone 71%, ds-DNA 63%).
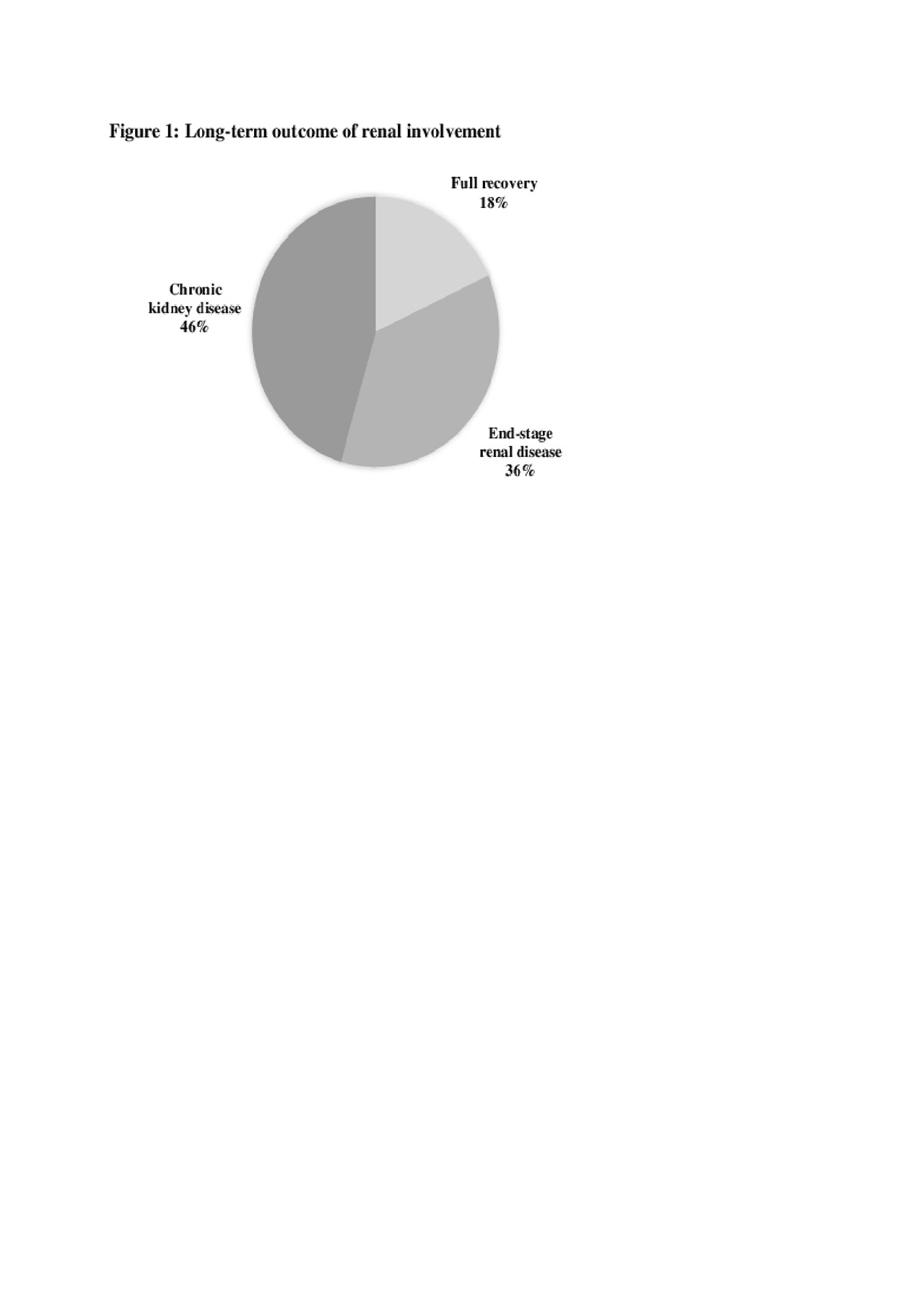
Median duration of follow-up was 30 months. One patient was lost to follow up, 4 patients (18%) had complete renal recovery and 18 patients (82%) had chronic kidney damage (Figure 1). Higher serum Creatinine and need for dialysis at onset of the disease were associated with worse outcome (p=0.002, p=0, 0046 respectively). Overall death in the cohort was 6 (26%) patients, 3 of whom died within the first year of diagnosis due to complications related to vasculitis. 7 patients (30%) had diffuse alveolar hemorrhage, while 4 (17%) had nodular opacities, with resolution of both entities on follow up testing.
Most commonly used treatments were systemic steroids (83%), cyclophosphamide (34%) and rituximab (26%). 19 patients (83%) received induction therapy. 12 patients (52%) received induction and short-term maintenance therapy, with a median duration of 6 months. 4 patients (18%) received induction and are still on maintenance therapy to date. 2 patients (8%) did not receive any treatment. No relapse or progression of kidney disease was noted in the whole cohort despite variable treatment regimens, including patients who did not receive any treatment.
Conclusion: HAV mainly involves the kidneys and the lungs. Renal outcome is poor regardless of induction or maintenance therapy regimens. No relapse occurred in our series, which represents the longest follow up to date. Maintenance therapy may not be needed in these patients. Cohorts with longer follow up duration are needed to validate this observation.
To cite this abstract in AMA style:
Almaaitah S, Yaseen K, Jin Y, Hajj-ali R. Long Term Outcome of Hydralazine-Associated Vasculitis [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/long-term-outcome-of-hydralazine-associated-vasculitis/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/long-term-outcome-of-hydralazine-associated-vasculitis/