Session Information
Date: Monday, November 13, 2023
Title: (1534–1553) Vasculitis – ANCA-Associated Poster II: Epidemiology, Outcomes, & Classification
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: There is limited data on the epidemiology and long-term outcome of patients with Interstitial Lung Disease (ILD) in ANCA-associated Vasculitis (AAV) with conflicting results regarding the effectiveness of the immunosuppressive treatment.
Methods: We retrospectively reviewed 1,002 patients with AAV or ANCA associated ILD followed at a single academic medical centre. ILD patients were those with chest CTs showing UIP, NSIP, organising pneumonia or chronic hypersensitivity pneumonia. We compared the occurrence of ILD with the presence and histology of nephritis, focusing on fibrotic phenotypes and assessed the impact of immunosuppressive therapy on the rate of evolution of FVC% and TLCOc% between treatment initiation (T0) and 12(±3) months (T12).
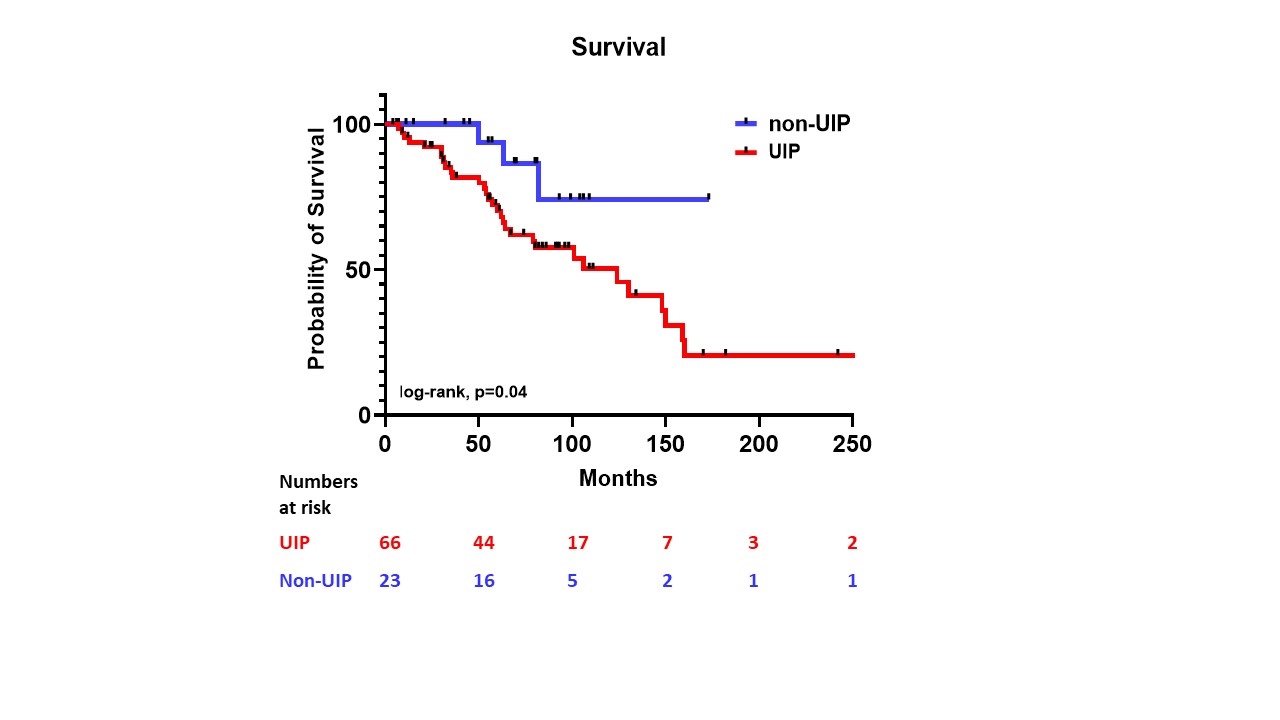
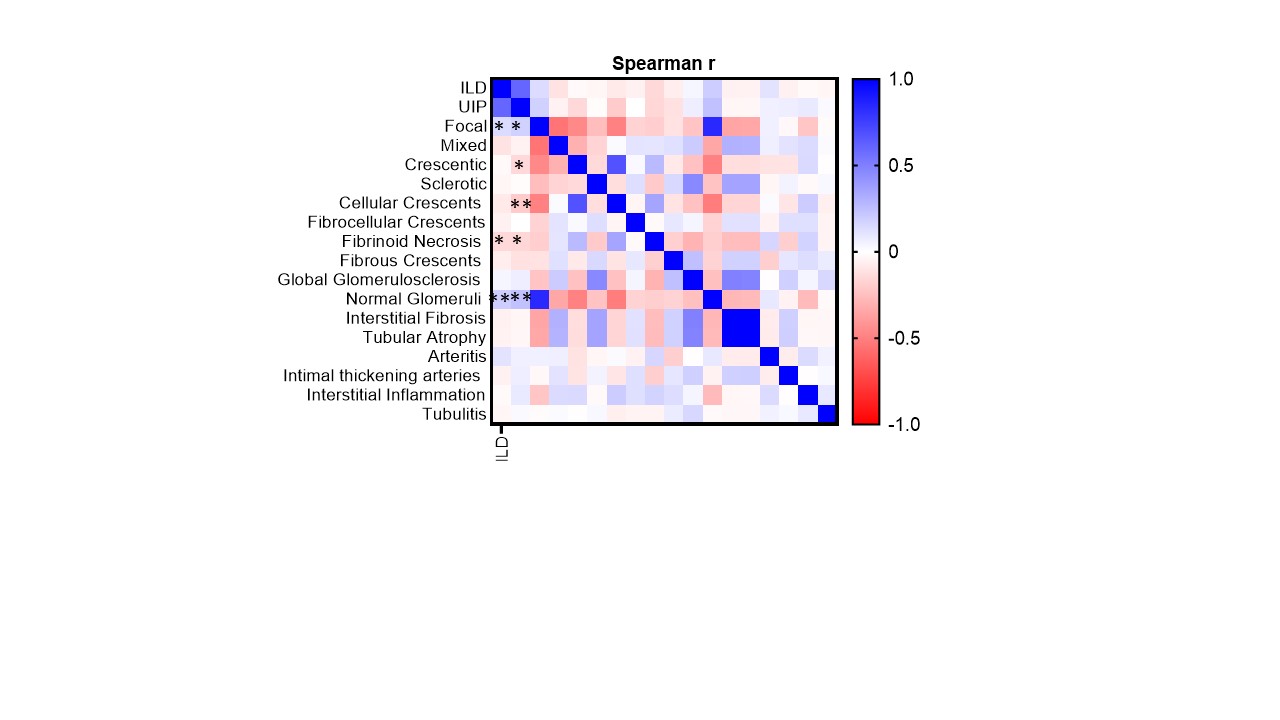
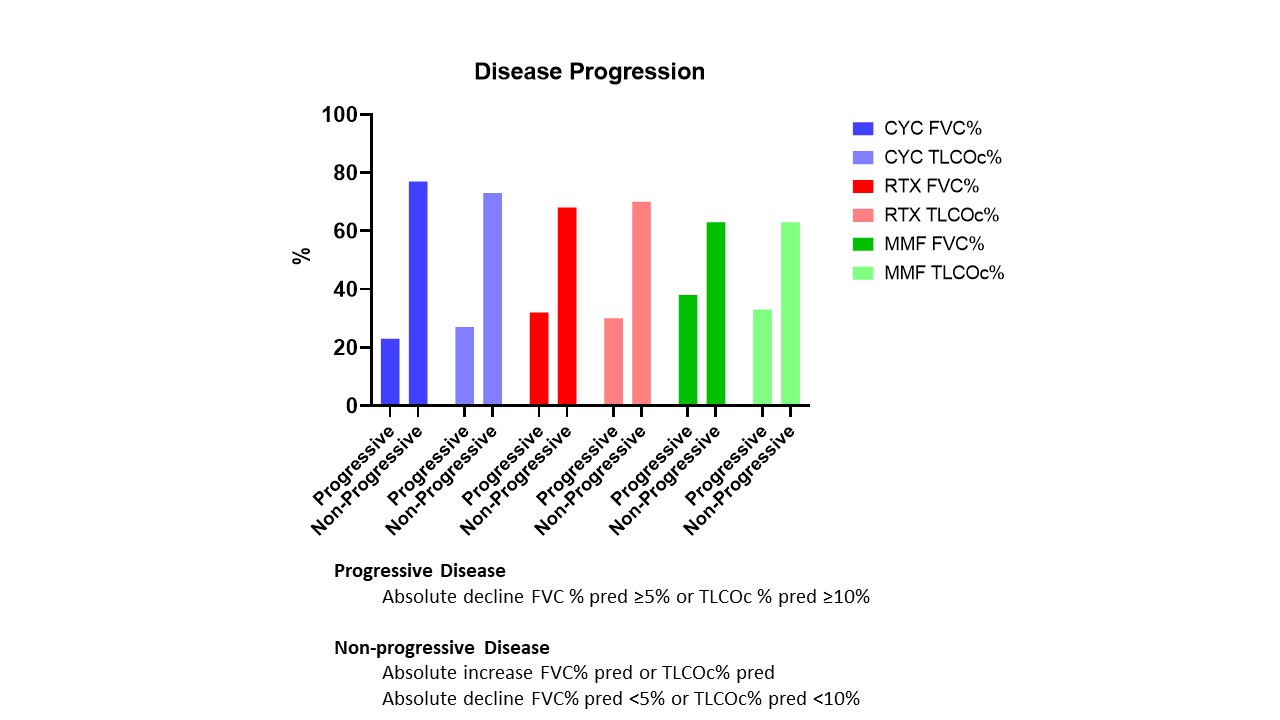
Results: 54 had microscopic polyangiitis (MPA; AAV-ILD), 15 had granulomatosis with polyangiitis (GPA; AAV-ILD) and 20 had ANCA positive ILD without vasculitis (ANCA-ILD). The total prevalence of ILD was 8.9% (n=89) with mean age 69.2±10.8 years and MPO positivity in 82%. In MPO cohort the prevalence of ILD was 19.6% and these patients presented higher ANCA levels [81.5±50.8 (ILD) vs 59.9±51 (non-ILD), p=0.002]. The median survival was 10 years; the survival with UIP (n=66) was worse compared to non-UIP (n=23) (log-rank, p=0.04, figure 1). No difference in survival between AAV and ANCA-ILD was found. Patients with AAV-ILD and renal involvement (n=47) had better kidney function and lower proteinuria at diagnosis compared to those with nephritis without ILD (n=186) (mean eGFR 41.87 vs 29.6 ml/min/1.73m2, p=0.007). The presence of ILD was also correlated with lower kidney histological activity (normal glomeruli r=0.193, cellular crescents r=-0.200, fibrinoid necrosis r=-0.151, all p< 0.05, figure 2), while the mixed class in ILD patients characterized with more interstitial fibrosis compared to mixed class in non-ILD (r=0.289, p=0.04) [total cohort 10y ESRD-free survival 91.3 (ILD) vs 82% (non-ILD)]. Median respiratory failure free-survival was 10 years and FVC% at baseline was an independent risk factor for respiratory failure (oxygen requirement) [HR 0.94 CI 95% (0.892-0.994), p=0.030]. When evaluating the impact of immunosuppression on lung progression over 12 months (cyclophosphamide, CYC, n=30; rituximab, RTX, n=25; mycophenolate, MMF, n=8) (figure 3), higher increase of FVC% and lower decline of TLOCc% were reported in the CYC compared to the RTX groups [mean difference: FVC%= -2.49, 95% CI (-10.06 to 5.07), TLCOc=-11.25, 95% CI (-33.08 to 10.58)].
Conclusion: We have reported the prevalence and long-term outcomes of AAV and ANCA associated ILD. Respiratory failure rates were similar between AAV-ILD and ANCA-ILD groups and dominated over ESKD in AAV-ILD. Kidney involvement in ILD presented with less glomerular abnormalities while the mixed class with more fibrotic features compared to patients without ILD. Within the limitations of this study, immunosuppressive treatment appeared to retard progression of lung disease in the short term.
To cite this abstract in AMA style:
chalkia a, Jones D, Sivasothy P, Jayne D. Long-term Observational Study of Interstitial Lung Disease in ANCA-associated Vasculitis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/long-term-observational-study-of-interstitial-lung-disease-in-anca-associated-vasculitis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/long-term-observational-study-of-interstitial-lung-disease-in-anca-associated-vasculitis/