Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Data from observational studies suggests a 10-12% biannual rate of progression from non-radiographic axial SpA (nr-axSpA) to ankylosing spondylitis (AS)1 in patients not treated with tumor necrosis factor α (TNF) blockers. It is not known, whether anti-TNF treatment might be able to prevent such a progression in patients with nr-axSpA. To assess the radiographic progression in the sacroiliac joints (SIJ) during long-term (up to 6 years) treatment with the TNF-blocker etanercept in patients with early axSpA.
Methods: In the ESTHER trial2 a total of 76 patients with early (=<5 years symptom duration) and active axSpA were randomized to be treated with either etanercept or sulfasalazine for one year. At year 1, all patients who were not in remission continued with etanercept directly; patients in remission discontinued their therapy and were followed-up until year 2, in case of disease flare the etanercept therapy was (re)-introduced and continued until the end of year 6. X-rays of SIJ were collected at baseline and every 2 years thereafter. Two trained readers (VRR and DP), who were blinded for all clinical data, scored independently the SIJ y-rays in a concealed and randomly selected order, according to the grading system of the modified New York (mNY) criteria for AS. Patients were classified as having AS if both readers recorded the presence of definite radiographic sacroiliitis according to the mNY criteria. Active inflammatory and fatty lesions on magnetic resonance imaging (MRI) of SIJ were assessed according to the Berlin MRI scoring system (KGH and CA).
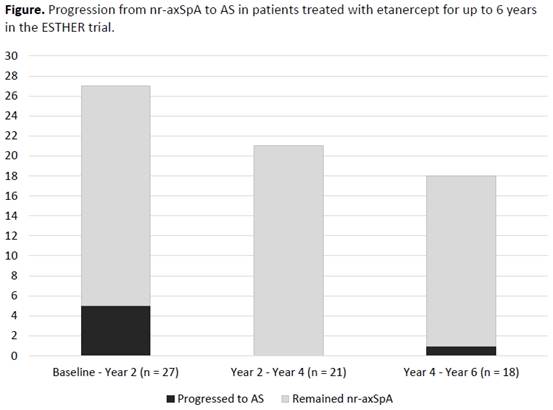
Results: A total of 55 patients from the 76 patients of ESTHER trial were included in the current analysis due to the availability of x-rays of SIJ. 19 patients (34.5%) were classified at baseline as AS and 36 (65.5%) as nr-axSpA based on the independent reading results with a fair agreement between both readers (k=0.33, p=0.01). Radiographic progression from nr-axSpA to AS was observed mainly between baseline and year 2 – in 18.5% (5/27) of the patients classified as nr-axSpA at baseline with available SIJ x-rays at year 2. There were no patients who progressed to AS between year 2 and year 4 and only one patient (5.6%, 1/18) progressed to AS between year 4 and year 6 – Figure. Treatment arm in the first year (etanercept or sulfasalazine) had no significant impact on progression from nr-axSpA to AS. Elevated C-reactive protein – CRP (>=5mg/l) at baseline was associated with a higher odds for progression: odds ratio = 7.0 (95%CI 0.7-73.9). There was no difference in the baseline osteitis score on MRI of SIJ between progressors and non-progressors (since MRI inflammation was an entry criterion), however, progressors had higher fatty lesions score at baseline as compared to non-progressors: 10.3±7.1 vs. 4.9±5.8, respectively, p=0.064.
Conclusion: In the ESTHER trial, there was a substantial reduction of radiographic sacroiliitis progression between year 2 and year 6 of anti-TNF treatment. Higher baseline CRP and higher MRI fatty lesions score demonstrated a positive association with progression from nr-axSpA to AS. References
1. Poddubnyy D, et al. Ann Rheum Dis 2011;70:1369-74.
2. Song IH, et al. Ann Rheum Dis 2011;70:590-6.
To cite this abstract in AMA style:
Rios Rodriguez V, Sieper J, Hermann KG, Haibel H, Althoff C, Buß B, Behmer O, Poddubnyy D. Long-Term Anti-TNF Treatment Is Associated with Reduction of Progression of Radiographic Changes in the Sacroiliac Joints in Patients with Non-Radiographic Axial Spa: Six-Year Results of the Esther Trial [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/long-term-anti-tnf-treatment-is-associated-with-reduction-of-progression-of-radiographic-changes-in-the-sacroiliac-joints-in-patients-with-non-radiographic-axial-spa-six-year-results-of-the-esther-tr/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/long-term-anti-tnf-treatment-is-associated-with-reduction-of-progression-of-radiographic-changes-in-the-sacroiliac-joints-in-patients-with-non-radiographic-axial-spa-six-year-results-of-the-esther-tr/