Session Information
Date: Saturday, November 16, 2024
Title: Patient Perspectives Poster
Session Type: Poster Session A
Session Time: 10:30AM-12:30AM
Background/Purpose: My journey with a rare, chronic, relapsing rheumatic disease began in November 2010 with a variety of seemingly unrelated symptoms: migrating joint pain, night sweats, sinus congestion, dyspnea, and chronic tussis. An episode of hemoptysis a year later led to surgery for subglottic stenosis (SGS). In January 2012, a rheumatologist diagnosed me with Granulomatosis with Polyangiitis (GPA). After my second hospitalization for a relapse, I received serial Rituximab (RTX).
Six years later, I made the joint decision with my doctor to halt RTX maintenance infusions. After 39 months, a slow-onset relapse required SGS surgery; then a CT scan showed lung nodules. Two months later, at the first of my two outpatient appointments for RTX, I was hospitalized with a PE. Re-infusion worked and I’m now on an RTX maintenance protocol.
Intervention: Throughout a world-wide pandemic, now in its fifth year, and with the specter looming of a possible outbreak of Highly Pathogenic Avian Influenza, I’ve fine-tuned my management of my disease toward being a “precision” patient. Reviewing well-vetted information allows me to focus appointments with my medical team.
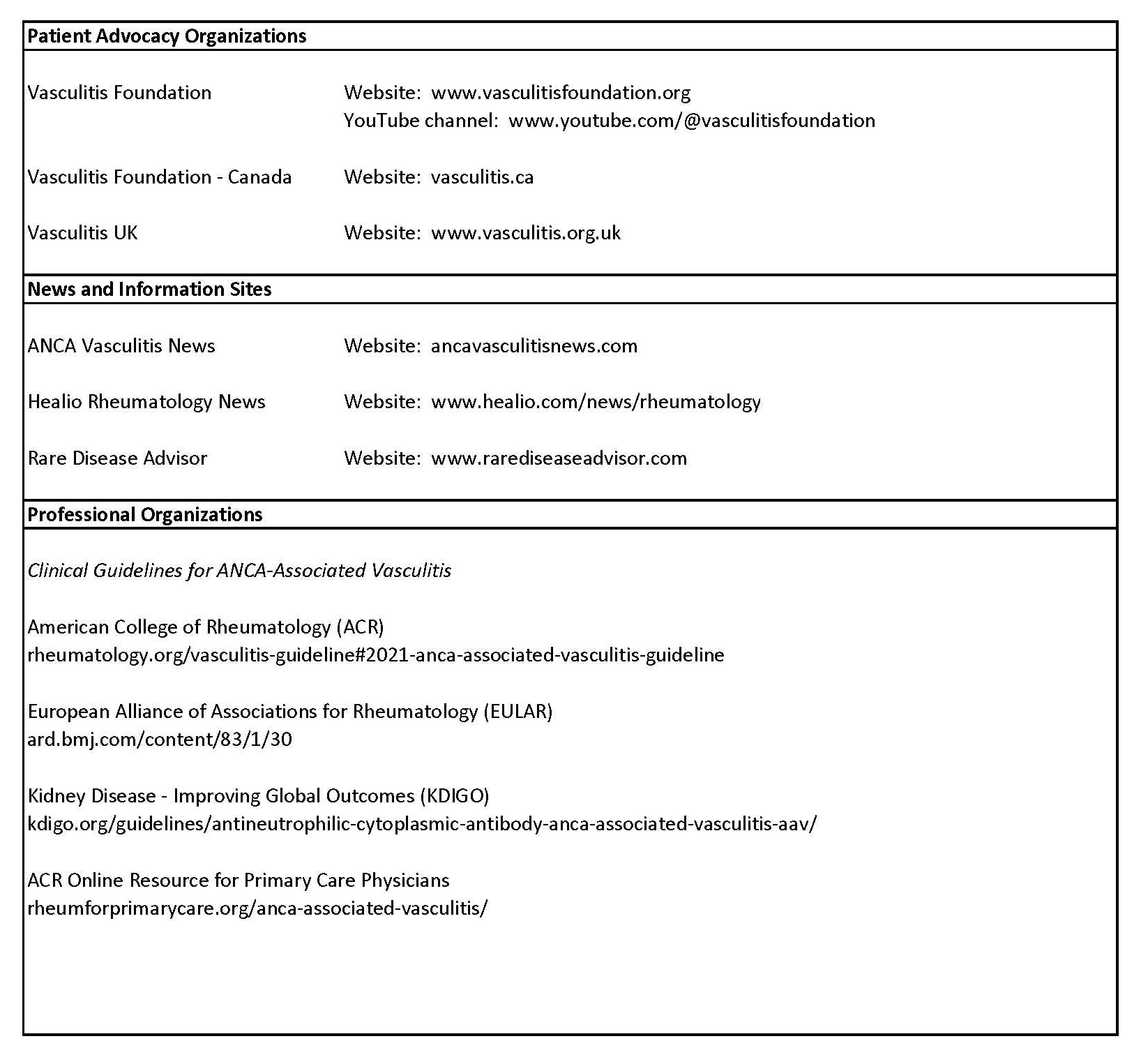
Key to my approach is keeping abreast of the latest medical information. Patient Advocacy Organizations, News and Information web sites, and Professional Organizations are valuable resources (Fig. 1). Information transforms me from being a passive recipient of what happens to being proactive about planning for what may occur.
Maintenance: Every 3-4 months, I have appointments with specialists to monitor my disease. Doctors have come and gone over the years, but fundamental to our work as a team is communication.
In a 2000 essay (1) titled “Can I Trust You?”, family physician Willam D. Hakkarinen outlines ways in which physicians could build trust with patients by “asking their opinions and considering their needs.” Written before the EHR explosion, the article provides simple ways doctors can elicit information from patients that provide benefits to both.
Primary care physician Michael Stein (Fig. 2) describes the patient-physician interaction in the context of chronic illness, noting the importance of kindness in its many forms. I resonate with his description of how chronic illness feels like a betrayal of one’s body. When I needed voice therapy to help with dysphonia, I recall telling my otolaryngologist that GPA was taking away another piece of my identity.
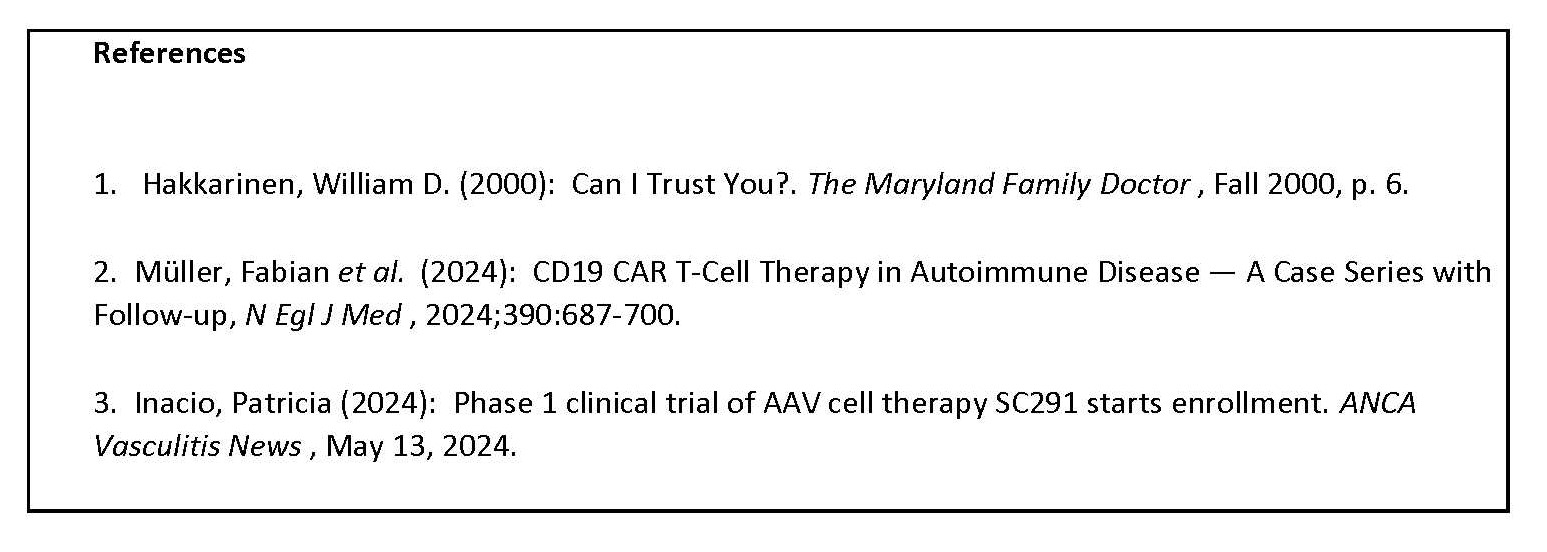
Quality of Life: Precision medicine for autoimmune diseases is on the horizon. A February 2024 paper (2) indicated CD19 chimeric antigen receptor T-cell therapy resulted in long-lasting remission to a small set of patients with three different autoimmune diseases. In May, a biotechnology company reported on recruitment (3) for a Phase I study of patients with hard-to-treat GPA or microscopic polyangiitis to receive CAR T-cell therapy. (All references listed in Fig. 3.)
While my disease has responded well to RTX re-infusion, knowing of the potential for targeted treatments for refractory disease is encouraging. New therapies that provide long-term, stable remission for vasculitis can provide renewed hope for many patients.
To cite this abstract in AMA style:
Hakkarinen I. Living Well with a Rare Rheumatic Disease – Becoming a “Precision” Patient on the Horizon of Precision Medicine [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/living-well-with-a-rare-rheumatic-disease-becoming-a-precision-patient-on-the-horizon-of-precision-medicine/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/living-well-with-a-rare-rheumatic-disease-becoming-a-precision-patient-on-the-horizon-of-precision-medicine/