Session Information
Date: Saturday, November 6, 2021
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster I: Diagnosis (0323–0356)
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
Background/Purpose: Lipoprotein(a) [Lp(a)] is a well-recognized, independent risk factor for atherosclerotic cardiovascular disease. Cardiovascular disease is one of the leading causes of death in patients with systemic lupus erythematosus (SLE). Indeed, women with lupus have 2.66 times increased risk compared to controls, with both SLE-specific and traditional cardiovascular risk factors playing a role. In this cross-sectional study, we evaluated Lp(a) levels in patients with SLE and evaluated for an association between atherosclerotic events, thrombotic events, renal disease, and disease activity.
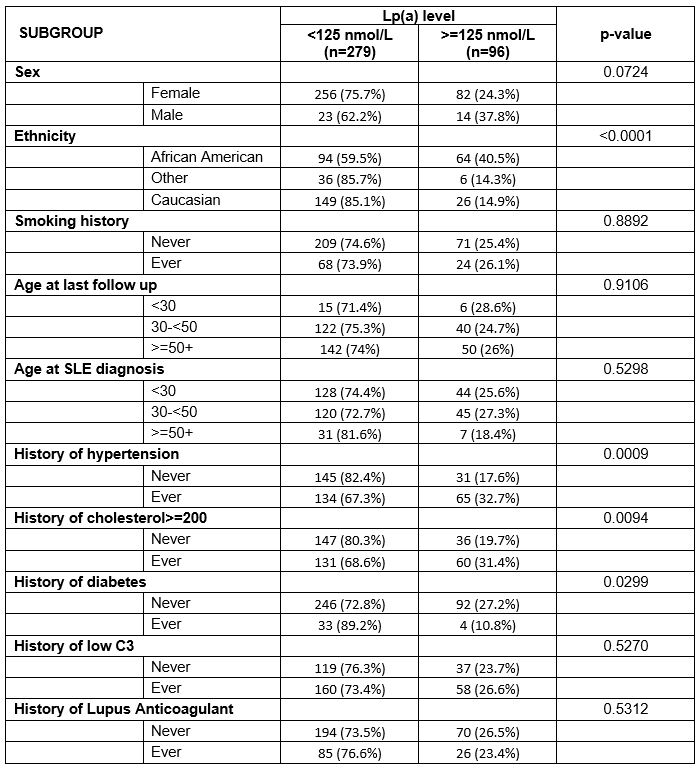
Methods: SLE patients fulfilling the revised American College of Rheumatology (ACR) or SLICC classification criteria with a measurement of Lp(a) were included in the analysis. A cutoff of 125 nmol/L was chosen based on expert opinion. Chi-square test was used to compare the differences between patient characteristics, including traditional and disease specific cardiovascular risk factors, and Lp(a) levels. Logistic regression or linear regression were used, where appropriate, to assess the association between Lp(a) values and the measured outcomes.
Results: 389 measurements of Lp(a), contributed from 375 patients were analyzed; 12 patients had 2 measurements and 1 had 3 measurements. Of these patients, 90% were female, 42% African American, and 47% Caucasian. The distribution of Lp(a) was heavily right skewed; values ranged from 8 to 671 nmol/L with a mean of 94 and median of 47nmol/L. Men, African American patients, patients with history of hypertension and hypercholesterolemia were more likely to have Lp(a) levels >=125 nmol/L. Patients with a history of diabetes were less likely to have levels >=125 nmol/L (Table 1).
In this study, we did not observe an association between Lp(a) and atherosclerotic or thrombotic events. There was an association between elevated Lp(a) level and a history of proteinuria (OR 1.78, p-value=0.026). This association remained significant following adjustment for age, sex, race, low C3, and elevated anti-dsDNA (OR=1.74, p-value=0.0498). There was also an association with eGFR< 60 (p=0.03). Patients with higher Lp(a) levels also had higher physician global activity (p=0.02).
Conclusion: Consistent with the general population, Lp(a) levels skewed toward lower values in patients with SLE. There was not an association between Lp(a) and atherosclerotic or thrombotic events, but this may have been limited due to small sample size. Elevated levels of Lp(a) were associated with proteinuria, reduced eGFR and physician global activity, with an inverse association observed with type 2 diabetes mellitus. An increase in Lp(a) concentrations has previously reported in non-SLE renal disease even prior to reduction in eGFR. The role of Lp(a) as a potential biomarker for early renal disease and poor renal outcomes in SLE warrants further evaluation with consideration for more granular subphenotyping.
To cite this abstract in AMA style:
Connolly C, Li J, Goldman D, Fava A, Magder L, Petri M. Lipoprotein(a) in Systemic Lupus Erythematosus Is Associated with History of Proteinuria and Renal Insufficiency [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/lipoproteina-in-systemic-lupus-erythematosus-is-associated-with-history-of-proteinuria-and-renal-insufficiency/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lipoproteina-in-systemic-lupus-erythematosus-is-associated-with-history-of-proteinuria-and-renal-insufficiency/