Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Cardio-pulmonary involvements of systemic sclerosis (SSc), including cardiomyopathy, interstitial lung disease, and pulmonary arterial hypertension (PAH) are leading causes of SSc-related deaths. Several potent effective PAH-specific therapies have recently been recently available, improving survival of patients with overall PAH. However, the survival of patients with PAH associated with SSc (SSc-PAH) is still poorer than that of patients with PAH associate with other connective tissue diseases (CTDs). To explore the characteristics relevant to poor survival of SSc-PAH patients, we analyzed hemodynamics data.
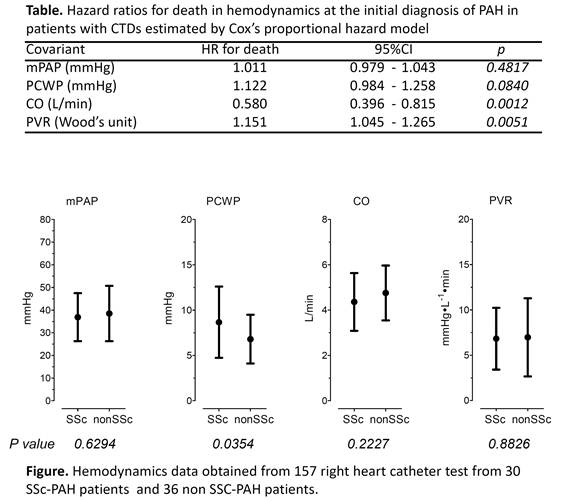
Methods: We analyzed 157 right heart catheter data obtained from 66 patients with PAH associated with CTDs, including 30 patients with SSc, and 36 non-SSc-CTD patients ( 17 patients with SLE,13 patients with MCTD and 6 patients with other CTDs), who had been followed between January 1980 and April 2012 in our hospital. We compared mean pulmonary artery pressure (mPAP), cardiac output (CO), pulmonary capillary wedge pressure (PCWP) and pulmonary vascular resistance (PVR) between SSc-PAH patients and non-SSc-PAH patients. Survival from the date of the initial diagnosis of PAH was measured, and analyzed using Cox’s proportional hazard model.
Results: The values (mean ± SD) of mPAP, CO, PCWP, and PVR at the initial diagnosis of PAH were 37.7 ± 11.3 mmHg, 4.6 ± 1.2 L/min, 7.7 ± 3.5 mmHg, and 6.9 ± 3.8 Wood’s units, respectively. Thirty-six of the 66 patients died. Cox’s proportional hazard model estimated that lower CO, higher PVR and higher PCWP, but not mPAP in hemodynamics at the initial diagnosis of PAH appeared to be risk factors for death (Table). Of the 36 patients who died, 20 were SSc-PAH patients. Moreover, PCWP measured throughout the course of PAH was significantly higher in SSc-PAH patients than that in non-SSc-PAH patients (8.66 ± 3.93 mmHg, 6.79 ± 2.73 mmHg, respectively; p=0.0354) (figure).
Conclusion : These results demonstrate that the presence of left ventricular diastolic dysfunction as evidenced by the elevation of PCWP plays a role in pathophysiology and poor prognosis of SSc-PAH. The data therefore suggest the importance of care for left ventricular diastolic dysfunction under management using PAH-specific therapies in order to improve prognosis in SSc patients.
Disclosure:
S. Tanaka,
None;
E. Ogawa,
None;
T. Wada,
None;
T. Nagai,
None;
J. Okada,
None;
S. Hirohata,
None.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/left-ventricular-diastolic-dysfunction-may-play-a-role-in-pathophysiology-and-poor-prognosis-of-pulmonary-arterial-hypertension-associated-with-systemic-sclerosis/