Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Given the nationwide shortage of rheumatologists, particularly in rural areas, many Veterans Affairs (VA) facilities have struggled to hire or retain specialists, resulting in greater reliance on non-VA (i.e., community-based) care. While non-VA care can expand access, it also increases costs for the VA and contributes to fragmented care for Veterans. To address these challenges, we launched the VA National Tele-Rheumatology Program (NTRP) in collaboration with the VA Office of Rural Health. In this study, we describe the implementation and early evaluation of the NTRP using the RE-AIM framework.
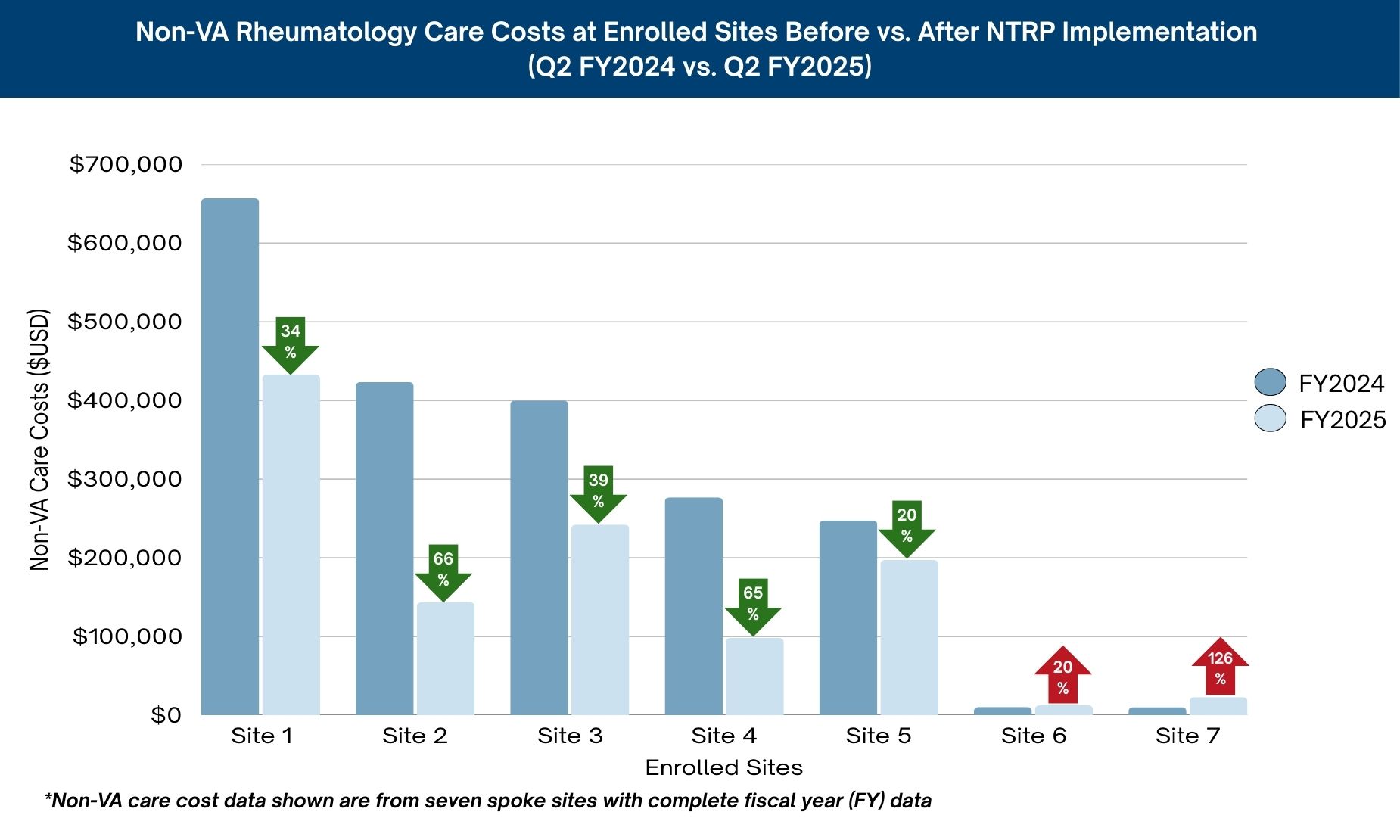
Methods: The NTRP is a centrally-managed and scalable telehealth model designed to deliver virtual rheumatology care across the country. The program launched in July 2024 with 3 clinical teams, each consisting of a rheumatologist and a Telehealth Clinical Technician with a shared nurse and pharmacist. The NTRP coordinates services and care delivery from a single site that triages and manages care for multiple outlying facilities. To recruit facilities into the program, NTRP leaders targeted sites with a high proportion of Veterans living in rural areas (according to Rural-Urban Commuting Area codes) and high expenditures on non-VA rheumatology care. Our initial evaluation used program records and data from the VA Corporate Data Warehouse to report on facility participation and characteristics (Adoption), Veteran enrollment and demographics (Reach), and non-VA care cost metrics (Implementation; Figure 1).
Results: Adoption: 13 facilities were recruited, most of which were located in the Southern U.S. (61.5%). Facility-level rurality ranged from 9.0% to 75.0% (Figure 2). Reach: 1,099 Veterans (83.2% male, 83.6% White, and mean (SD) age of 63.6 (15.1) years) received care through NTRP, 47.6% of whom lived in rural or very rural areas. Implementation: Among 7 enrolled sites with complete cost data, non-VA care expenditures for rheumatology care in Quarter 2 (Q2) of Fiscal Year (FY) 2024 averaged $289,361. These expenditures dropped by 43.2% in Q2 FY2025 (Figure 3).
Conclusion: In its first year, NTRP had significant adoption and reach across rural geographies. Early evaluation suggests that non-VA care expenditures rapidly decrease at participating facilities. Although we anticipate that the NTRP will lead to reduction in total costs for rheumatology care, additional evaluation is needed to determine whether savings in non-VA care outweigh the costs of NTRP implementation and maintenance, and whether these cost reductions are sustained over time. Future work will also assess additional clinical and maintenance outcomes according to the RE-AIM framework.
 RE-AIM Domains, Measures, and Strategies Used in the NTRP
RE-AIM Domains, Measures, and Strategies Used in the NTRP
.jpg) Geographic Distribution of VA Sites Enrolled in the NTRP as of Q2 FY2025
Geographic Distribution of VA Sites Enrolled in the NTRP as of Q2 FY2025
.jpg) Non-VA Rheumatology Care Costs at Enrolled Sites Before vs. After NTRP Implementation (Q2 FY2024 vs. Q2 FY2025)
Non-VA Rheumatology Care Costs at Enrolled Sites Before vs. After NTRP Implementation (Q2 FY2024 vs. Q2 FY2025)
To cite this abstract in AMA style:
Wilson C, Nasrallah C, Tarasovsky G, Hamblin A, Williams A, Flynn B, Ng B, Schmajuk g. Launch of the National Tele-Rheumatology Program (NTRP) to Expand Rheumatology Care to Rural Veterans [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/launch-of-the-national-tele-rheumatology-program-ntrp-to-expand-rheumatology-care-to-rural-veterans/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/launch-of-the-national-tele-rheumatology-program-ntrp-to-expand-rheumatology-care-to-rural-veterans/
