Session Information
Session Type: Abstract Session
Session Time: 4:00PM-5:30PM
Background/Purpose: : Immune checkpoint inhibitors (ICI) for cancer treatment can cause inflammatory arthritis (IA). ICI-IA is a heterogeneous entity affecting peripheral joints, tendons, and rarely the axial skeleton, and can be severe and persist even after ICI cessation. Since ICI-IA is a distinct entity with unique pathogenesis, applying categories of traditional IA is limited; thus, we used a data-driven approach to define clinically relevant subgroups within ICI-IA and examined differences between subgroups.
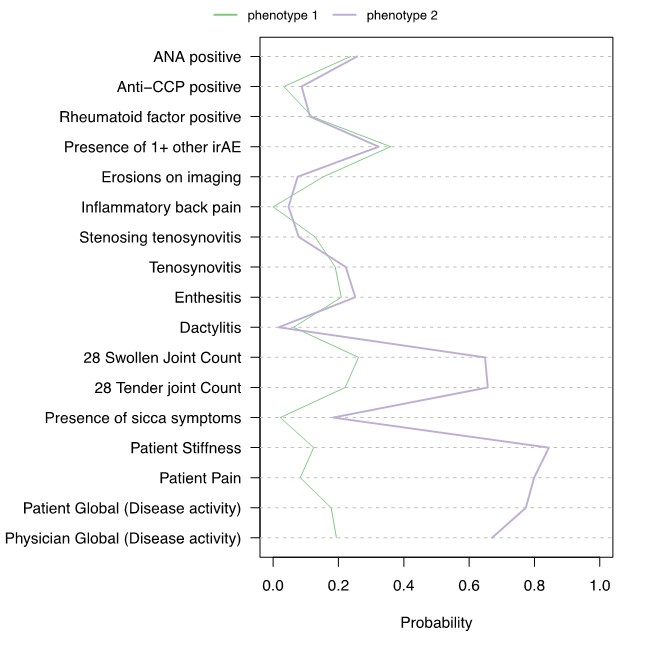
Methods: Participants were ³18 years old, treated with anti-PD-1, anti-PD-L1, and/or anti-CTLA-4 agents alone or in combination, and had ICI-IA diagnosed by a rheumatologist. We used information from the baseline rheumatology visit (patient reported symptoms, physical exam features, physician global arthritis rating, and laboratory studies) to cluster patients with latent class analysis (LCA). The Bayesian Information Criteria (BIC) was used to select the number of phenotypes with the lowest BIC. We then compared demographics, cancer type and treatments, and IA treatments and outcomes between the estimated phenotypes. Next, we estimated the association between these features of interest and the likelihood of being in the group with the most severe IA symptoms using logistic regression.
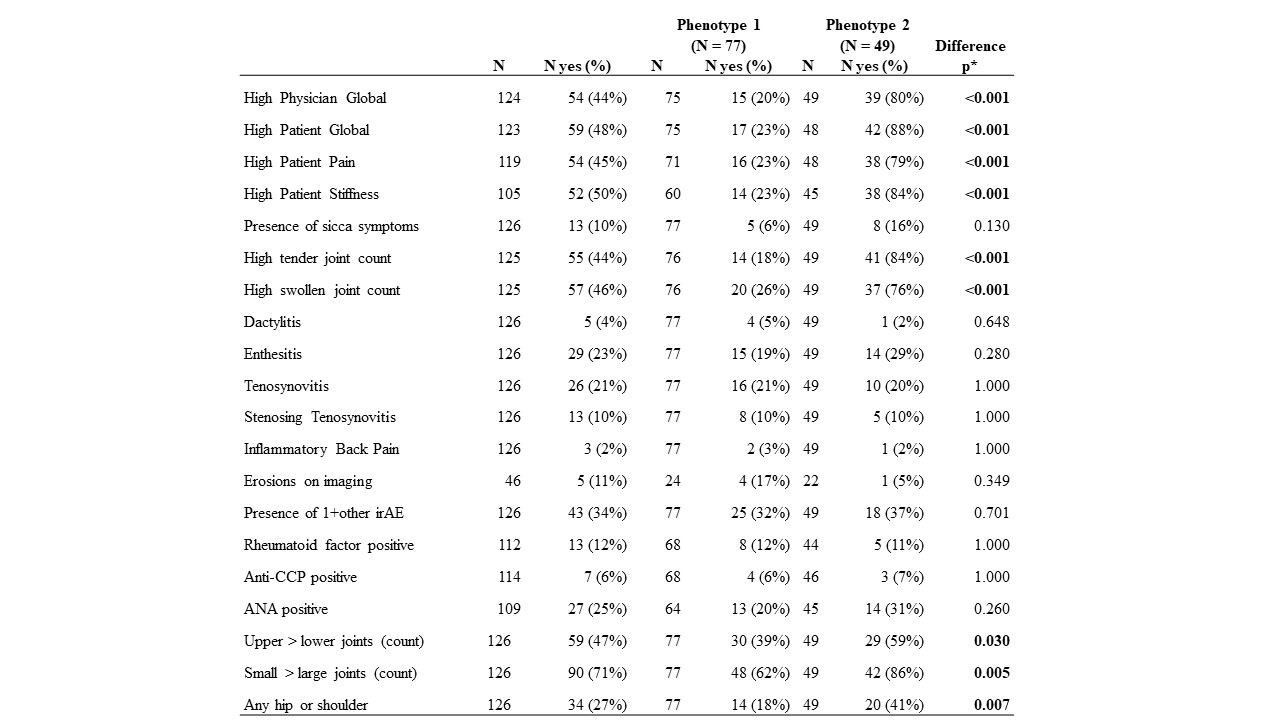
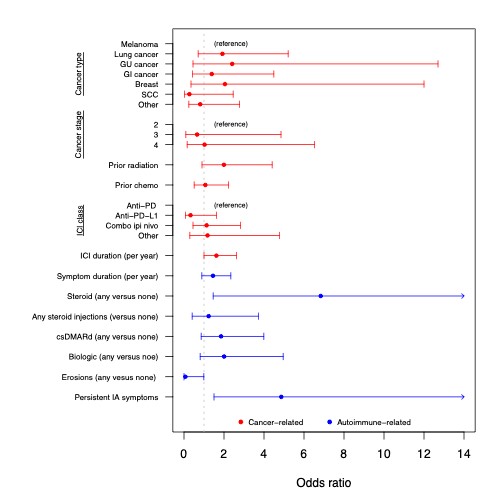
Results: Of the 126 patients with ICI-IA, most participants were female (56%) and white (92%). Most patients had a moderate or high disease activity by CDAI. Mean CDAI was 16.98 (SD 10.2). Twenty variables were used to estimate latent classes. Two distinct phenotypes were indicated by the BIC; 77 patients are estimated to be the first phenotype and 49 in the second phenotype (Figure 1). The significantly different features of the phenotypes included higher levels of all components of the CDAI, more stiffness, and having more small and upper extremity joints involved for phenotype 2 (Table 1). Anti-CCP and RF positivity did not differ between groups. Patients in phenotype 2 were more likely to require steroids as compared to patients in phenotype 1 and were more likely to have persistent IA >6 months after ICI cessation (Figure 2). There was also a trend of longer ICI exposure prior to ICI-IA in phenotype 2, but no association with type of ICI or cancer.
Conclusion: Two separate phenotypes of ICI-IA were identified using LCA, the second having a more severe polyarthritis at baseline affecting the upper extremities. Those in the group with more severe features at baseline were more likely to need corticosteroids and to have persistent IA. There were no differences in terms of cancer type and treatment, thus future research can interrogate underlying genetic and immunologic differences between groups.
To cite this abstract in AMA style:
Cappelli L, Perin J, Bingham C, Shah A. Latent Class Analysis Identifies 2 Clinical Phenotypes of Immune Checkpoint Inhibitor-induced Inflammatory Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/latent-class-analysis-identifies-2-clinical-phenotypes-of-immune-checkpoint-inhibitor-induced-inflammatory-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/latent-class-analysis-identifies-2-clinical-phenotypes-of-immune-checkpoint-inhibitor-induced-inflammatory-arthritis/