Session Information
Session Type: Poster Session B
Session Time: 5:00PM-6:00PM
Background/Purpose: Juvenile Idiopathic Arthritis (JIA) is the most common chronic rheumatic disease in childhood, affecting 1 to 22 per 100,000 children. JIA-associated uveitis is known to occur in up to 12% of JIA patients in the United States. Visual complications are present in up to 2/3 of patients, with blindness in as many as 30-50% of affected eyes. The gold standard to diagnose JIA-associated uveitis is slit lamp examination by trained eye specialists using a subjective grading scale (Standardization of Uveitis Nomenclature or SUN) to quantify anterior segment inflammation. Recently, laser flare photometery (LFP) has been used in multiple studies as an objective, non-invasive, and quantitative method to measure anterior chamber inflammation. LFP has been used by ophthalmologists to monitor JIA-associated uveitis patients as well as other forms of pediatric non-infectious chronic anterior uveitis.
The purpose of this study is to investigate if LFP can be used in a pediatric rheumatology office setting to diagnose patients with JIA-associated uveitis.
Methods: This observational study was approved by the Phoenix Childrens IRB, and enrolled patients aged 4-16 years diagnosed with JIA based on the 2001 ILAR classification criteria during 2019-2022. Exclusion criteria were having a history of JIA-associated uveitis or any other form of uveitis, as well as history of pacemaker placement. All patients underwent at least one evaluation of both eyes using a Kowa FM-600 laser flare photometer, as well as a standard slit lamp examination by optometry or ophthalmology during routine clinical care. Data collected at patient visits included demographics, JIA characteristics, treatment medications, LFP readings, and AC cell grade scored by SUN grading system. Data were summarized using descriptive analyses and the uveitis false positive rate was calculated along with 95% confidence interval.
Results: Subjects included 58 pediatric patients diagnosed with JIA with data obtained for 138 eyes at 69 visits. The mean age was 8.4 years (range: 1.2-16.3 years) at diagnosis and 11.9 (range: 4.8-16.5) years at enrollment. Of the 58 patients, the majority 43 (74.1%) were female (table 1). Most common JIA subtypes included 19 (32.8%) patients with persistent oligoarticular JIA, and 12 (20.7%) with RF negative polyarticular JIA. At enrollment, 15 patients (25.9%) were on no medications, with 26 (44.8%) on methotrexate, 22 (37.9%) on adalimumab, 6 (10.3%) on tocilizumab, and 5 (8.6%) on etanercept (table Treatment at baseline included methotrexate (44.8%), adalimumab (37.9%), etanercept (8.6%), tocilizumab (10.3%) and none (25.9%) (table 2). During the study period, no eye exams detected active uveitis based on slit lamp exam with a SUN grade over 0. However, of the 135 LFP readings, 131 (97.0%) were normal, yielding a false positive rate of 3% (95% CI of 0.8%, 7.4%) (table 3).
Conclusion: Laser Flare Photometry is a non-invasive tool that can be utilized in the pedaitric rheumatology clinic to evaluate for JIA-associated uveitis. There is a low false positive rate of LFP when compared with standard slit lamp exam. Future studies will examine LFP to monitor uveitis activity in patients with JIA-associated uveitis to help guide treatment decisions.
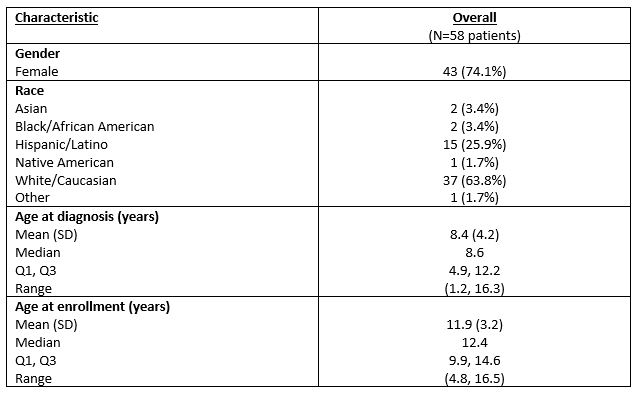 Table 1. Demographic characteristic data at baseline
Table 1. Demographic characteristic data at baseline
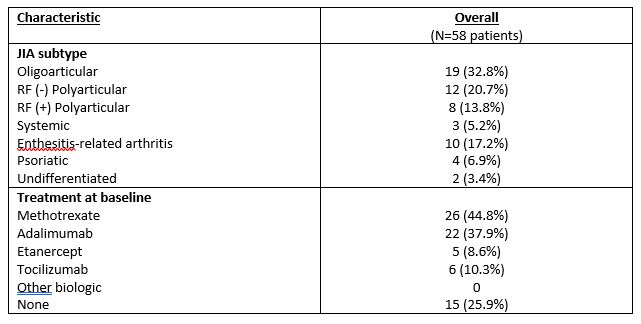 Table 2. JIA subtype and treatment characteristic data at baseline
Table 2. JIA subtype and treatment characteristic data at baseline
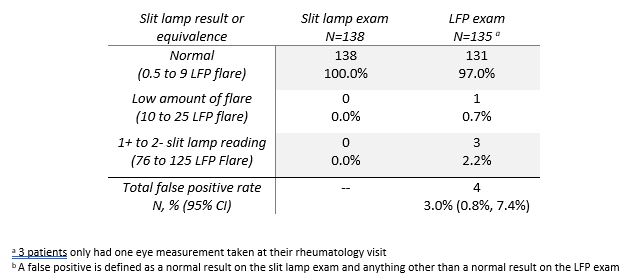 Table 3. Uveitis activity based on slit lamp exam versus Laser Flare Photometry (LFP)
Table 3. Uveitis activity based on slit lamp exam versus Laser Flare Photometry (LFP)
To cite this abstract in AMA style:
Ede K, Shishov M, Wershba E, Goswami N, Gorry S, Jospeh M, Mirea L, O'neil J. Laser Flare Photometery in the Pediatric Rheumatology Clinic as a Screening Tool for Juvenile Idiopathic Arthritis Associated Uveitis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/laser-flare-photometery-in-the-pediatric-rheumatology-clinic-as-a-screening-tool-for-juvenile-idiopathic-arthritis-associated-uveitis/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/laser-flare-photometery-in-the-pediatric-rheumatology-clinic-as-a-screening-tool-for-juvenile-idiopathic-arthritis-associated-uveitis/
