Session Information
Date: Tuesday, November 14, 2023
Title: (2387–2424) Vasculitis – Non-ANCA-Associated & Related Disorders Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Manifestations of giant cell arteritis (GCA) include large vessel involvement (LVI) of the aorta and its branches. Aortic aneuryms are more common compared to the general population. GCA is complicated by an increased risk of infections, likely due to treatment and/or the systemic nature of the disease. There is limited information on the impact of the disease phenotype on the risk of infection among patients with GCA. No previous study has investigated LVI in GCA as a risk factor for severe infections. Such investigations need to take into account demographics and comorbidities. The objective of this study was to assess the influence of age, sex, LVI and pre-existing comorbidities on the risk of severe infection in GCA.
Methods: Patients with biopsy-proven GCA, diagnosed between 2002 and 2010, were identified from a regional pathology register, and followed through the end of study December 2011.
Data on infections requiring hospitalization were obtained from linkage to the regional healthcare registry. Twenty categories of infections were identified based on ICD-10 codes.
Five categories of pre-existing comorbidities were based on diagnoses registered within four years before the date of GCA diagnosis, and the Charlson comorbidity index (CCI) was calculated. Information on LVI was obtained through structured review of all relevant radiological and clinic-physiological studies. LVI was defined as presence of aneurysm, ectasia, or stenosis of the aorta and/or its main branches or positive 18fluoro-2-deoxy-d-glucose positron emission tomography–computed tomography or other nuclear imaging methods indicating vasculitis. Patients with LVI findings after or ≤1 year before the GCA diagnosis were classified as having the LVI phenotype. Cox regression analysis was used to identify possible predictors of severe infections among patients with GCA. Patients were followed from time of GCA diagnosis and censored at death or migration from the region. Covariates were excluded from multivariate models based on co-linearity.
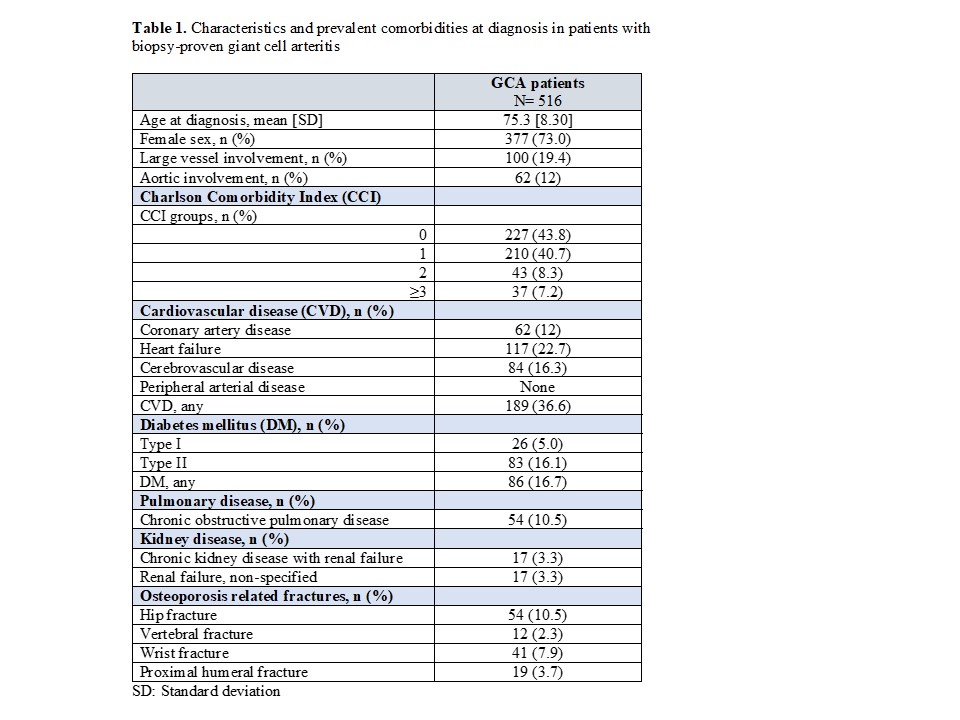
Results: Among 516 patients with biopsy-proven GCA (Table 1), 19.4% had confirmed LVI, and 12% had aortic involvement (aneurysm, ectasia, dissection or signs of vasculitis on nuclear imaging) with or without concomitant distributary artery affection. There were 118 patients with ≥1 severe infection during the study period.
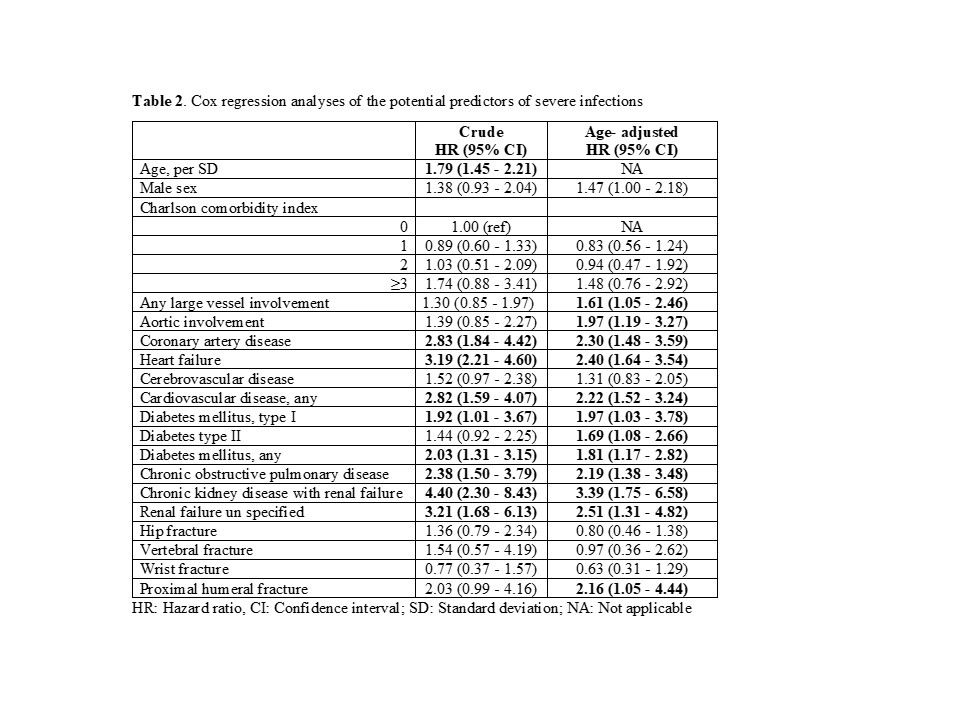
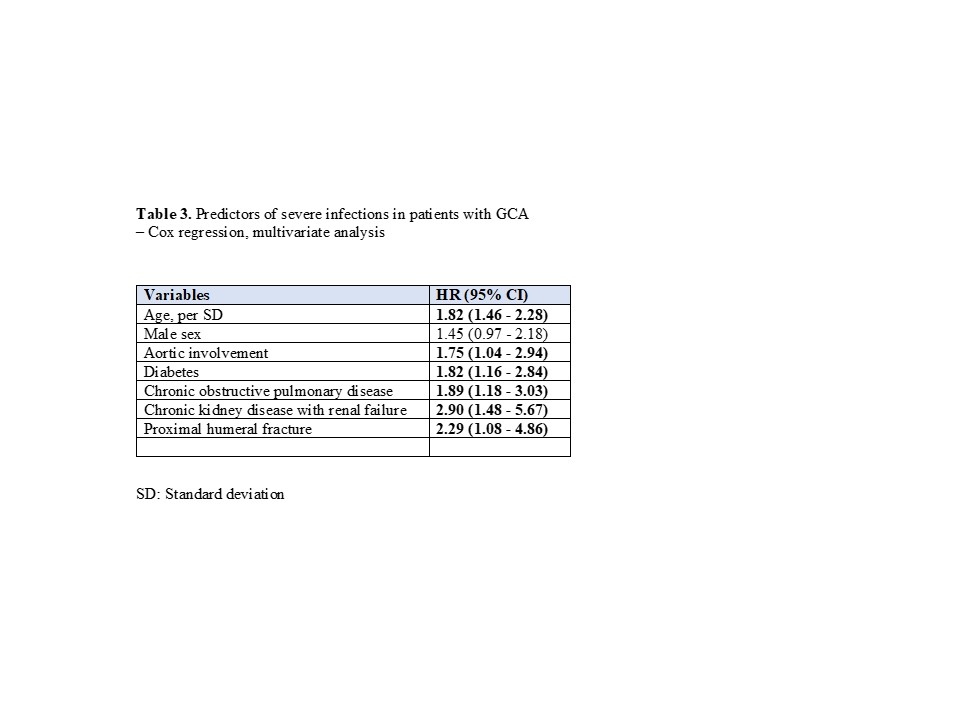
Higher age at diagnosis and several pre-existing comorbidities, i.e. coronary artery disease, heart failure, diabetes, chronic obstructive pulmonary disease and renal failure were significant predictors for severe infections (Table 2). LVI overall and aortic involvement were associated with significantly increased risk of severe infections in age-adjusted analyses (Table 2). In the multivariate analysis, aortic involvement was predictive of severe infections (Hazard ratio 1.75; 95% confidence interval 1.04-2.94, adjusted for age and comorbidities) (Table 3).
Conclusion: In patients with GCA, age and specific pre-existing medical conditions are predictors of severe infections. LVI, in particular of the aorta, may also be associated with a higher risk for severe infection.
To cite this abstract in AMA style:
Naderi N, Mohammad A, Wadström K, Bergström U, Turesson C. Large Vessel Involvement and the Risk of Severe Infections in Patients with Giant Cell Arteritis – a Population-based Study [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/large-vessel-involvement-and-the-risk-of-severe-infections-in-patients-with-giant-cell-arteritis-a-population-based-study/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/large-vessel-involvement-and-the-risk-of-severe-infections-in-patients-with-giant-cell-arteritis-a-population-based-study/