Session Information
Date: Tuesday, November 15, 2016
Title: Systemic Lupus Erythematosus – Clinical Aspects and Treatment - Poster III: Biomarkers and Nephritis
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Lupus nephritis (LN) class III or IV is associated with a poor prognosis for both patient and renal survival. The guideline or recommendation for LN has been recently established by both ACR and EULAR, and changing therapies is recommended for patients who do not respond adequately to the induction therapy for preventing damage accrual. However, it remains major challenge to determine when to switch the treatment. In this study, we determined appropriate period and targeted clinical status to switch the treatment in patients with an inadequate response in lupus nephritis class III or IV.
Methods: Eighty patients with biopsy-proven lupus nephritis class III or IV were retrospectively recruited and divided into 2 groups, with complete renal response (CR) or non-CR at 3 years after induction therapy. We investigated when clinical responses were obtained at each observational period from the baseline to year 3. Clinical responses were divided into 3 groups, CR, partial renal response (PR), and non-PR according to EULAR recommendation. Furthermore, patients were assessed by SDI, SLEDAI, and cumulative dose of corticosteroid for 3 years.
Results: Forty-four patients with CR and 36 with non-CR were enrolled. Cumulative CR rate was 85.0%. There is no significant difference in baseline clinical characteristics other than higher SLEDAI in patients with CR compared to those with non-CR (p<0.01). PR rates of patients with CR were significantly higher than those with non-CR from week 12 (p<0.01). We identified the achievement of PR at 12 weeks as an independent predictor (Odds ratio 3.57, p=0.03) by multivariate analysis. We next divided all patients into 2 groups according to PR achievement at week 12. The cumulative CR rate of the patients who achieved PR at week 12 was significantly higher than those who did not (96.5% vs 69.2%, p<0.001) (Figure1A). Moreover, a significantly higher SDI (Figure 1B) and cumulative dose of corticosteroid were seen in the patients who did not achieve PR at week 12 than those who did regardless of their CR status at year 3.
Conclusion: Lack of PR at week 12 predicts a lower likelihood of achieving CR at 3 years. Since achievement of PR at week 12 leads to less damage accrual without regard to CR status at year 3, switching treatment should be recommended for patients who failed to achieve PR at week 12 to reduce accrual of damage. 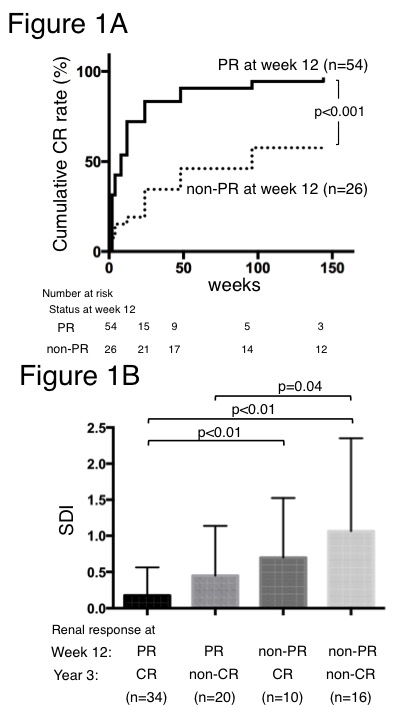
To cite this abstract in AMA style:
Hanaoka H, Yamada H, Kiyokawa T, Iida H, Suzuki T, Yamasaki Y, Ooka S, Nagafuchi H, Okazaki T, Ichikawa D, Shirai S, Shibagaki Y, Koike J, Ozaki S. Lack of Partial Renal Response By 12 Weeks after Induction Therapy Is an Indicator to Switch the Treatment in Lupus Nephritis Class III or IV for Reducing Future Damage Accrual [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/lack-of-partial-renal-response-by-12-weeks-after-induction-therapy-is-an-indicator-to-switch-the-treatment-in-lupus-nephritis-class-iii-or-iv-for-reducing-future-damage-accrual/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lack-of-partial-renal-response-by-12-weeks-after-induction-therapy-is-an-indicator-to-switch-the-treatment-in-lupus-nephritis-class-iii-or-iv-for-reducing-future-damage-accrual/
