Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Inflammatory back pain (IBP) is the defining feature of axial spondyloarthritis (axSpA). However, it may be difficult for non-rheumatology physicians (non-rheums) to distinguish between mechanical and inflammatory back pain (IBP) thus contributing to delayed and missed diagnosis. This study aims to systematically survey non-rheums in the US to gain insights into their knowledge, awareness, and attitudes towards IBP. The objective is to identify barriers for timely referral and opportunities for intervention.
Methods: An online survey questionnaire was developed and refined using input from previous smaller regional studies, methodologies, and pilot testing. The survey included demographic information, practice patterns, and questions about the knowledge and approach toward IBP and axSpA. The survey was distributed to non-rheums taking care of chronic back pain (CBP) patients, namely Family/Internal Medicine, Spine Surgery/Orthopedics, Pain Medicine, and Physical Medicine/Physiatry/Rehabilitation across the US using third-party vendors. The survey was also sent to rheumatologists (rheums), who served as the comparator group. Descriptive statistics was used to summarize the results.
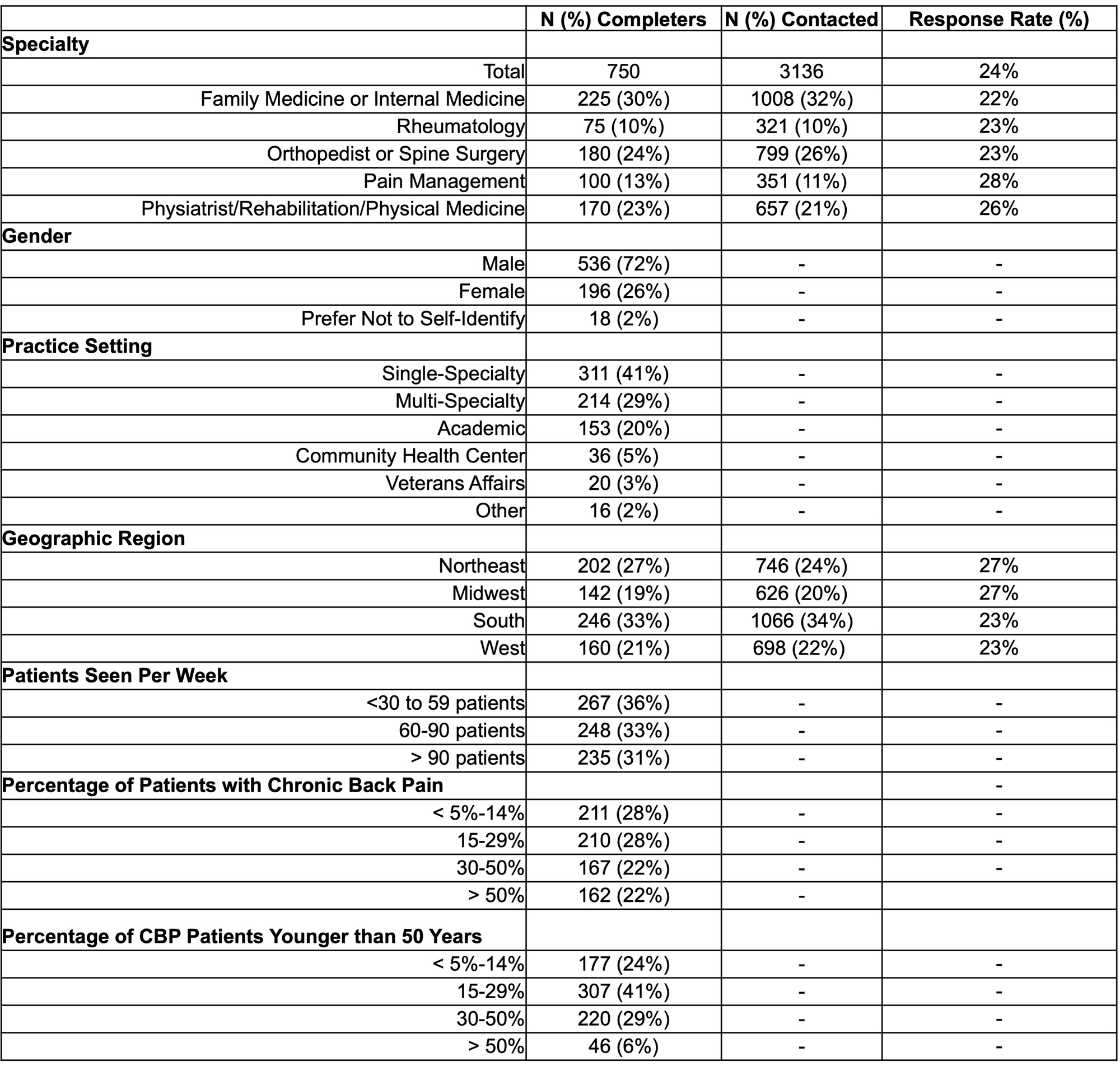
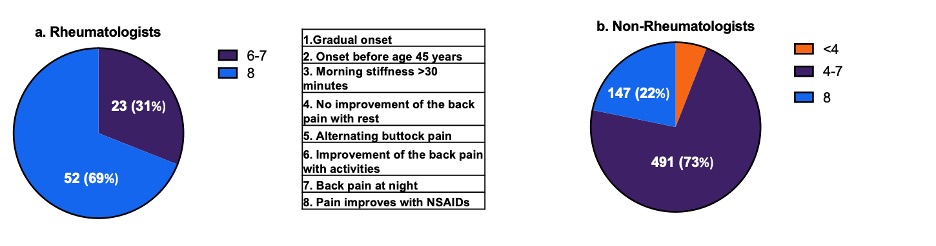
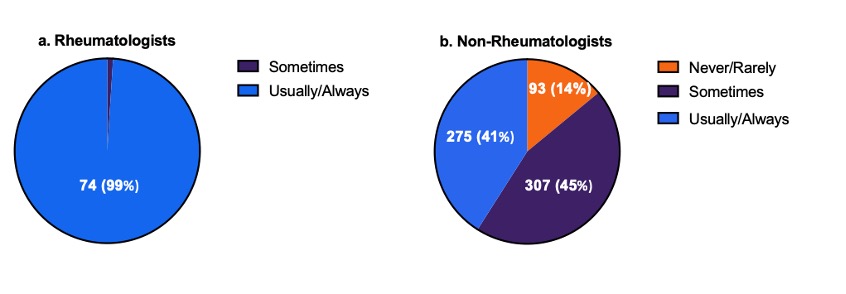
Results: Of 3136 physicians who received the survey, 750 completed it (response rate 24%). Table 1 presents information regarding physician specialty, demographics, and practice details. Physicians with variable years of practice experience were included (40% < 5-15 years, 40% 15-30 years, and 10% > 30 years). Respondents reported CBP as a common symptom among the patients; 72% of physicians reported CBP in 15% of their patients and 44% in 30% of patients. Seventy percent of non-rheums reported that 15 to 50% of their CBP patients have onset before age 50 years. About 75% of non-rheums are either moderately or very familiar with the term IBP; an additional 15% are somewhat familiar. Only 21% of non-rheums could identify all 8 IBP items, but 87% could recognize more than 4 of 8 IBP items (Figure 1). Among rheums, 69 % could recognize all eight features, and 27% could recognize 7 of 8 features. About 60% of non-rheums do not routinely assess CBP patients for IBP; 14% rarely/ never assess, and 45% assess for IBP sometimes (Figure 2). In contrast, 99% of rheums are routinely assessed for IBP. Data about the IBP and response rates remained consistent across the non-rheums surveyed.
Conclusion: In this large nationwide survey study involving physicians from different specialties who manage CBP, we found that non-rheums are familiar with the term IBP, and the majority may have optimal knowledge about the IBP items, but fewer actually assess the CBP patients for the presence of IBP in routine practice. The use of computerized Clinical Decision Support Systems (CDSS) and improved education regarding the true prevalence of axSpA may help to wind down this barrier.
To cite this abstract in AMA style:
Odell W, Alexander S, Page N, Maheshwari N, Danve A. Knowledge, Awareness, and Attitudes Regarding Inflammatory Back Pain Among Non-Rheumatology Physicians in the United States [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/knowledge-awareness-and-attitudes-regarding-inflammatory-back-pain-among-non-rheumatology-physicians-in-the-united-states/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/knowledge-awareness-and-attitudes-regarding-inflammatory-back-pain-among-non-rheumatology-physicians-in-the-united-states/