Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: While the hip and knee are linked biomechanically, the risk of hip osteoarthritis (OA) in persons with knee OA has not been well studied. Knee OA is associated with weak hip girdle muscles which may predispose to hip OA. Furthermore, persons with painful knee OA may alter their gait and abnormally load other lower extremity joints. We examined the risk of hip OA in those with knee OA in the Multicenter Osteoarthritis Study (MOST).
Methods: MOST is a NIH funded cohort study of risk factors for knee OA. To evaluate hip OA, we used long limb films which included hip imaging obtained at baseline and 60 months follow-up. Radiographic hip OA was defined using the modified Croft definition, and we defined incident radiographic hip OA as development of OA at 60 months. To evaluate knee OA, PA and lateral weight bearing films were obtained at baseline. A knee had radiographic OA if that knee had either tibio-femoral or patello-femoral OA (Kellgren and Lawrence score >=2). Symptomatic knee OA was defined as knee with radiographic OA and knee pain on most days in a month. For the 1st analysis, the exposure groups were knees with or without (either unilateral or bilateral) radiographic knee OA at baseline. For the 2nd analysis, the exposure groups were knees with or without symptomatic knee OA at baseline. The outcomes for both analyses were incident radiographic hip OA. For both analyses, we compared the risk of incident radiographic hip OA in hips with or without (radiographic or symptomatic) knee OA. The analyses were adjusted for hip OA risk factors including age, sex, BMI, knee injury/surgery. We carried out subanalyses among those with unilateral prevalent radiographic and symptomatic knee OA to compare the risk of incident ipsilateral vs contralateral hip OA at 60 months.
Results: In the 1st analysis, the risk of incident radiographic hip OA with any radiographic knee OA was not significantly greater than risk of incident radiographic hip OA without any radiographic knee OA (see table 1). For the 2nd analysis, there was an increased risk of incident radiographic hip OA with any symptomatic knee OA (see table 1), and this increased risk was limited to the subset of subjects with unilateral symptomatic knee OA (adjusted OR 1.99, p = 0.01). Among those with prevalent radiographic or symptomatic knee OA, we found no predilection for ipsilateral vs. contralateral incident hip OA (see table 2).
Conclusion: Pre-existing radiographic knee OA did not increase risk for incident radiographic hip OA, but symptomatic knee OA may increase risk for incident radiographic hip OA. 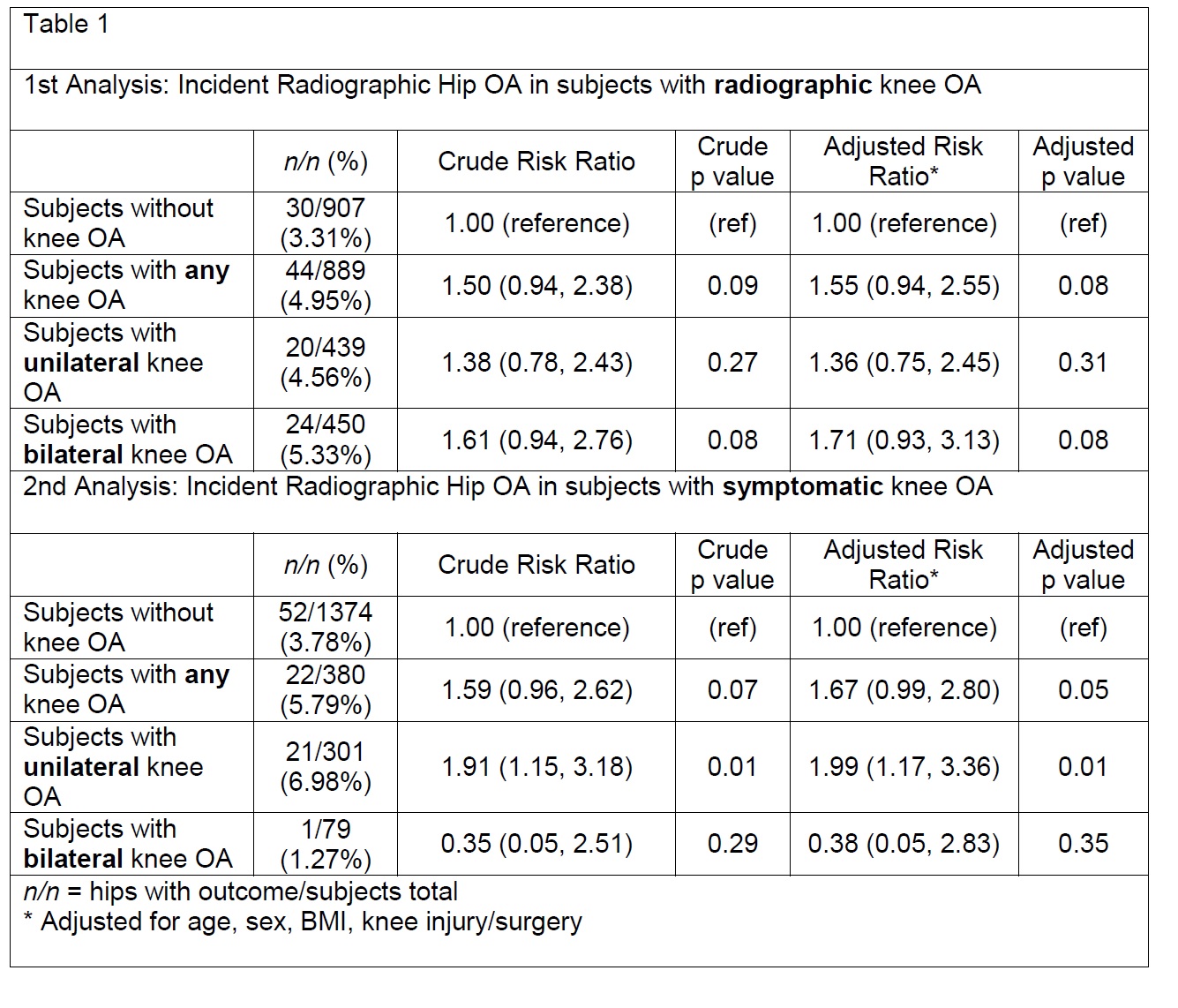

To cite this abstract in AMA style:
Kim C, Sheehy S, Lewis C, Clancy MM, Nevitt MC, Torner J, Lewis CE, Guermazi A, Felson DT. Knee Osteoarthritis As Risk for Hip Osteoarthritis [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/knee-osteoarthritis-as-risk-for-hip-osteoarthritis/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/knee-osteoarthritis-as-risk-for-hip-osteoarthritis/
