Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Interstitial lung disease (ILD) is a leading cause of mortality in scleroderma, underscoring the critical demand for reliable biomarkers. KL-6 and IL-18, have been investigated as potential lung-specific biomarkers in different types of ILD,
including systemic sclerosis (SSc) however, their predictive significance for ILD detection, progression and association with mortality remains unclear. The study aimed to assess the discriminative capabilities of serum biomarkers KL-6 and IL-18 in differentiating between various grades of fibrosis identified through semiquantitative CT extension in systemic sclerosis-associated interstitial lung disease (SSc-ILD). Additionally, we sought to compare the diagnostic performance of these biomarkers with traditional pulmonary function tests (FVC% and DLCO%) and to evaluate the significance concerning ILD progression and
short-term lung volume changes and mortality
Methods: We conducted a prospective and longitudinal investigation, including patients diagnosed with systemic sclerosis based on the 2013 ACR/EULAR criteria. Baseline and follow-up measurements at 12-18 months of chest high-resolution computed tomography (HRCT) scans and pulmonary function tests were retrieved. The annualized rate of change in forced vital capacity (FVC%) from baseline to follow-up served as a surrogate outcome for ILD progression. Serum concentrations of KL-6 and IL-18 were quantified using established quantitative ELISA techniques. We examined the sensitivity and specificity of various cut-off values of serum KL-6, IL-18, %DLCO, and %FVC annualized change for predicting survival.
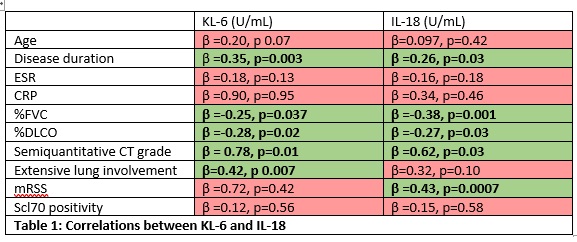
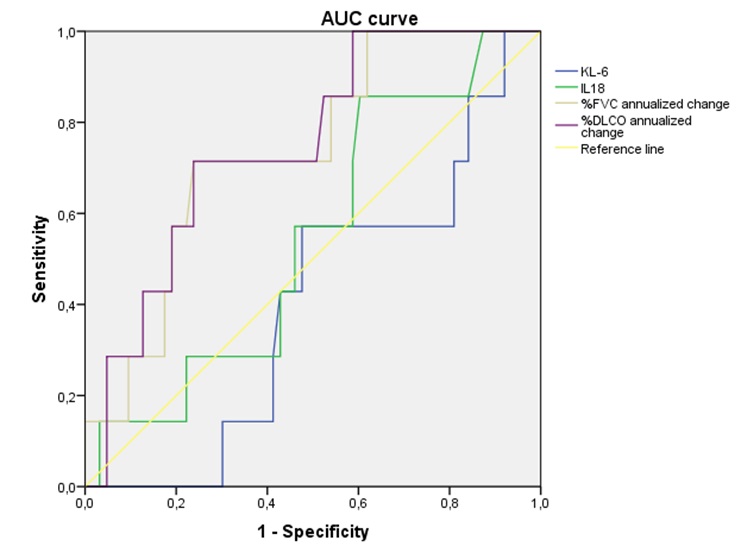
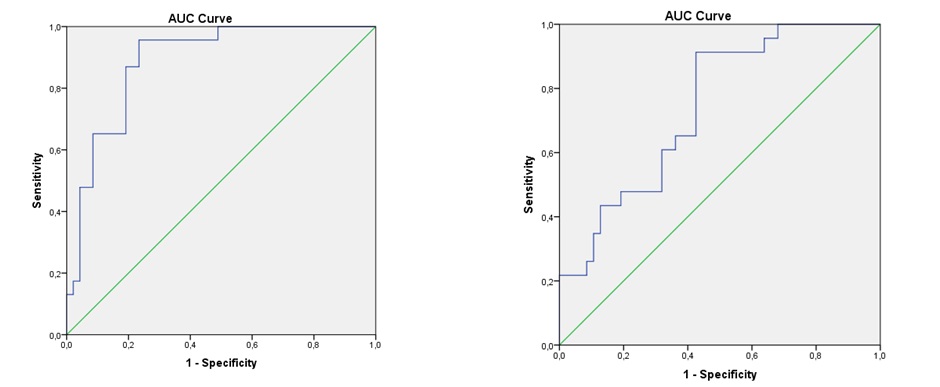
Results: A correlation was found between semiquantitative CT grade and serum levels of KL-6 (β=0.78, p=0.01) and IL-18 (β=0.62, p=0.03) (table 1). Receiver operating characteristic (ROC) analysis established optimal cut-off values for serum KL-6 (273.80 U/mL) and IL-18 (290.83 U/mL) in detecting ILD presence. The area under the curve (AUC) values for KL-6 and IL-18 outperformed FVC% and DLCO%, particularly in discriminating grade 2 from grade 1 ILD. During follow-up, 7 patients (9.5%) died. FVC% change ranged from −28% to 24%, and DLCO% change ranged from -38% to 28% Higher KL-6 levels at baseline were predictive of faster %FVC decline (β=-0.34, p=0.006) and %DLCO (β=-0.24, p=0.04) at 1-year follow-up (figure 1). Higher IL-18 levels at baseline were
predictive of faster %FVC decline (β=-0.24, p=0.04) but not %DLCO decline. A significant correlation between mortality and KL-6 (β=0.32, p=0.003), %DLCO (β=0.57, p=0.003), and %FVC (β=0.62, p=0.002) was found. %DLCO showed the best performance in predicting mortality compared to the other biomarkers. ROC analysis showed 668.34 U/mL as the KL-6 serum concentration for predicting mortality in SSc patients (figure 2).
Conclusion: Our study highlights KL-6 and IL-18 as robust predictors of ILD progression in SSc, with independent associations with short-term lung volume changes. Notably, %DLCO emerges as a superior predictor of mortality compared to KL-6 and IL-18, offering a valuable tool for risk stratification in SSc patients.
KL-6 (AUC=0.45, 95% CI 0.21–0.50; P=0.04), IL_18 (AUC=0.59, 95% CI 0.34–0.75, P=0.69), %FVC-annualized change (AUC=0.75, 95% CI 0.56-0.91, p=0.04), %DLCO-annualized change (AUC=0.75, 95% CI 0.58-0.92, p=0.03)
To cite this abstract in AMA style:
sieiro santos c, Retuerto M, Sierra L, Calleja Antolín S, Bollo de Miguel E, Ordas Martínez J, Pérez García P, Baenas P, Moriano Morales C, de la Calle Lorenzo J, Díez Álvarez E. KL-6 and IL-18 Biomarkers in Systemic Sclerosis-associated Interstitial Lung Disease: Enhancing Prognostic Insights into Early Detection, Progression, Lung Volume Changes,and Mortality Risk [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/kl-6-and-il-18-biomarkers-in-systemic-sclerosis-associated-interstitial-lung-disease-enhancing-prognostic-insights-into-early-detection-progression-lung-volume-changesand-mortality-risk/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/kl-6-and-il-18-biomarkers-in-systemic-sclerosis-associated-interstitial-lung-disease-enhancing-prognostic-insights-into-early-detection-progression-lung-volume-changesand-mortality-risk/