Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: The last few years have seen the approval of many new agents for the treatment of psoriatic arthritis (PsA) and psoriasis (PSO), resulting in greater options for managing moderate to severe disease. Many of these newer agents (guselkumab, upadacitinib, risankizumab) have been approved for both PSO and PsA.
As such, dermatologists’ biologic armamentarium closely parallels that of rheumatologists. With many PSO patients progressing to include joint involvement, managing joint disease has become more important. Most dermatologists are more confident in their ability to manage PsA without rheumatologists than in the past, with a subset further agreeing they treat patients for longer periods of time.
Methods: An independent market analytics firm collaborated with US rheumatologists and dermatologists in 2021 and 2022 to conduct a retrospective chart review of PsA patients who were recently switched from one advanced treatment to another (2022: 219 rheumatologists, 998 patient charts and 113 dermatologists, 510 patient charts. 2021: 203 rheumatologists, 1,022 patient charts and 157 dermatologists, 510 patient charts) in the prior twelve weeks. Physicians were able to submit up to seven patient charts. Data included patient demographics as well as physician demographics and attitudinal survey responses.
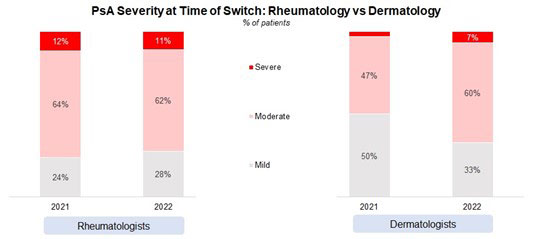
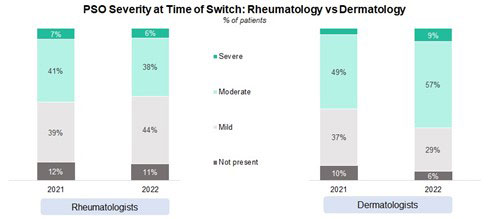
Results: Rheumatologist-treated patients have a more severe form of PsA when compared to those treated by dermatologists. However, more dermatologists are treating moderate and severe PsA when compared to 2021. PSO severity also tends to be higher among dermatologist-treated patients.
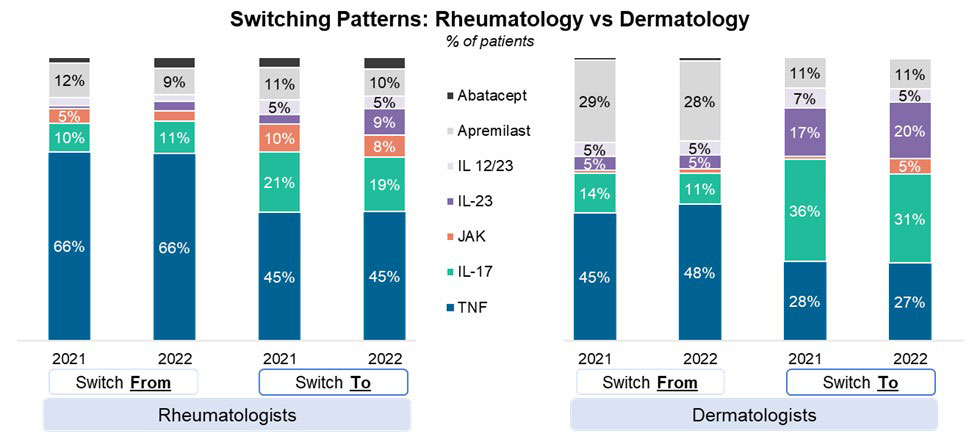
Switching patterns have remained relatively stable when compared to 2021 with Dermatologists reporting substantially greater switches from apremilast than rheumatologists. Rheumatologists were more likely to switch patients to TNFs when compared to dermatologists, with dermatologists reporting a higher incidence of switching to IL-17s and IL-23s. Rheumatologists switching patients to JAKs is lower than in 2021.
The level of co-management between the two specialties also varies. More dermatologists indicate co-management with a rheumatologist than those reported by a rheumatologist. Substantially more rheumatologists also report making the decision to switch patients without input from the dermatologist than the converse.
Conclusion: There exists several differences in the ways rheumatologists and dermatologists care for PsA patients. While dermatologists tend to see milder cases, they are primarily focused on treating skin manifestations, but the availability of a wider treatment armamentarium also means they are becoming more comfortable in treating other manifestations and therefore are more likely to feel confident in treating patients for longer periods of time before involving rheumatologists.
Rheumatologists are primarily concerned with treating joint disease and are more likely to refer to dermatologists in cases of uncontrolled skin manifestations. Rheumatologists are also less likely to involve dermatologists in treatment than vice-versa.
To cite this abstract in AMA style:
Yarnall M. Key Differences Between US Rheumatologists’ and Dermatologists’ Management of Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/key-differences-between-us-rheumatologists-and-dermatologists-management-of-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/key-differences-between-us-rheumatologists-and-dermatologists-management-of-psoriatic-arthritis/