Session Information
Session Type: Poster Session A
Session Time: 6:00PM-7:00PM
Background/Purpose: Relapsing polychondritis (RPC) is a rare multisystemic autoimmune disease associated with recurrent, progressive inflammation in cartilaginous structures. In children, the most common manifestations are auricular chondritis, arthritis, and respiratory tract involvement, with some studies reporting increased severity of laryngotracheal complications compared to adults. Given the paucity of literature describing RPC in pediatrics, this retrospective chart review aims to provide additional data on five patients regarding clinical presentation, management, and outcomes.
Methods: With approval by our institutional review board, we retrospectively reviewed the clinical presentation, management, and outcomes of patients clinically diagnosed with RPC before 18 years of age at Texas Childrens Hospital between January 2004 and December 2022. The diagnosis was defined according to the modified McAdams criteria. We reported the Relapsing Polychondritis Disease Activity Index (RPDAI) scores at the initial and final clinic visits. Remission was defined as having less than 2 exacerbations per year.
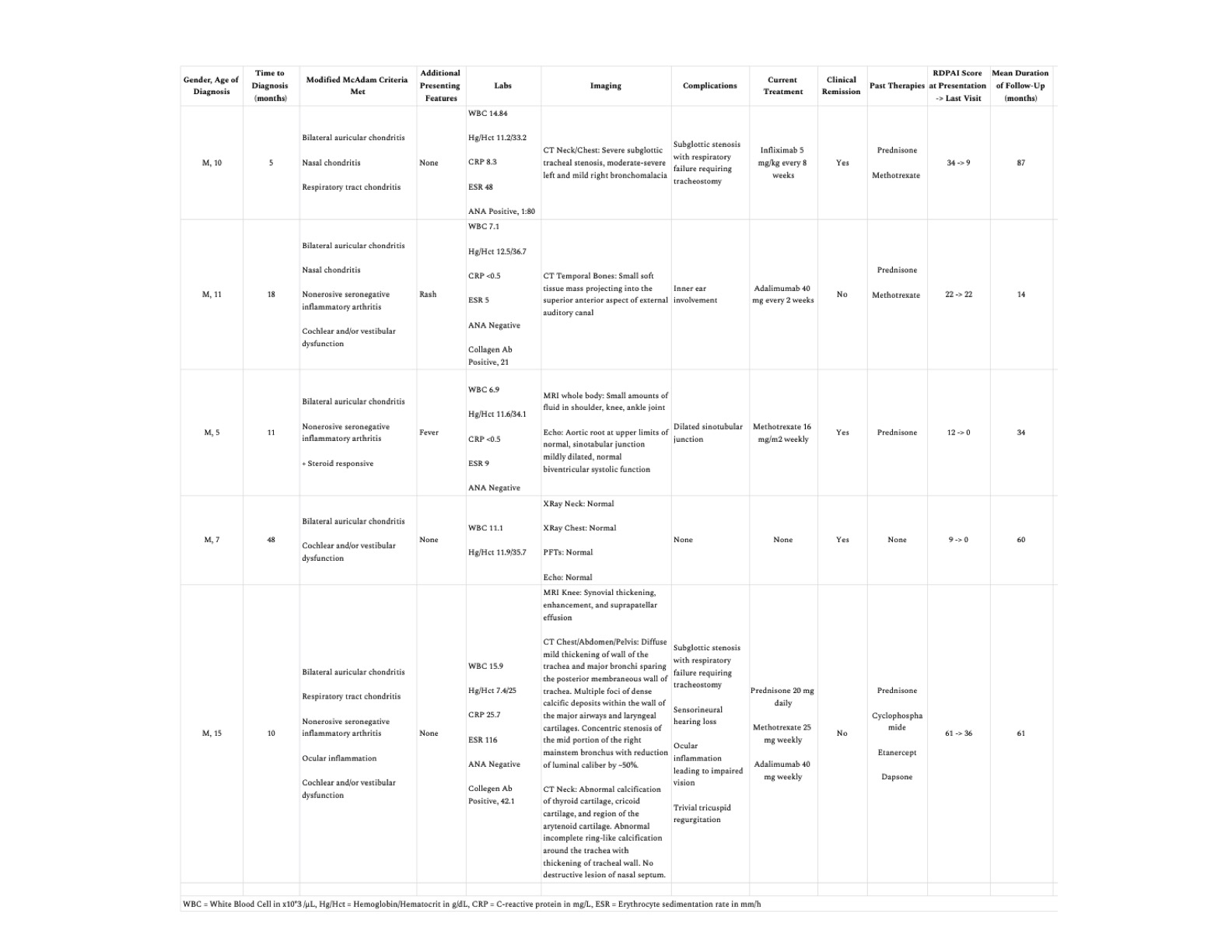
Results: Of the five patients diagnosed with RPC, all were male, with a mean age of 9.6 years (range: 5-15 years) at presentation. The mean time to diagnosis was 18.4 months (range: 5-48 months). All patients had auricular chondritis, which was the presenting complaint for 4. Inflammatory arthritis was the next most common symptom in 3 patients, followed by nasal and bronchial chondritis in 2 and 1 with ocular involvement. The clinical presentations and initial labs/imaging are summarized in Table 1.
Two patients with tracheal chondritis presented in acute respiratory failure requiring emergent tracheostomy. One had dense calcific deposits on CT with resultant bronchial stenosis, and the other had evidence of bronchomalacia. A patient who reported vertigo during episodes of auricular chondritis underwent a CT temporal bone that revealed a soft tissue mass projecting into the external auditory canal. Two others developed conductive and sensorineural hearing loss. None developed a saddle nose deformity. Evaluation of cardiac manifestations noted one patient with mild aortic sinotubular junction dilation and another with tricuspid regurgitation. The mean RDPAI index on presentation was 27.6 (range: 9-61) and decreased by 48% from the first to the last visit.
Of the four patients who received treatment, all were given prednisone and methotrexate. Three patients received additional immune modulation, including anti-TNF agents and cyclophosphamide. Three achieved clinical remission. One patient required no therapy and remains in remission after five years. No secondary systemic autoimmune diseases were identified, or deaths reported.
Conclusion: Relapsing polychondritis is a rare autoimmune disease in children with variable severity, clinical course, and response to treatment. In our cohort, none developed a concomitant systemic autoimmune disease. Treatment with immunosuppression resulted in a decrease in RPDAI scores and clinical remission in 60%. Additional prospective studies are needed to determine the optimal treatment course and the validity of RPDAI for use in clinical practice.
To cite this abstract in AMA style:
Chun A, Molina S, De Guzman M, Pereira Palacios M. Juvenile Relapsing Polychondritis: A Single Center Cohort [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 4). https://acrabstracts.org/abstract/juvenile-relapsing-polychondritis-a-single-center-cohort/. Accessed .« Back to 2023 Pediatric Rheumatology Symposium
ACR Meeting Abstracts - https://acrabstracts.org/abstract/juvenile-relapsing-polychondritis-a-single-center-cohort/