Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: Physicians strive to provide patient-centered, timely care, often with perceived inadequate blocked time on the schedule. We aim to understand the joint injection workflow, its time allocation in the clinic, and physician satisfaction with the process in our academic rheumatology center.
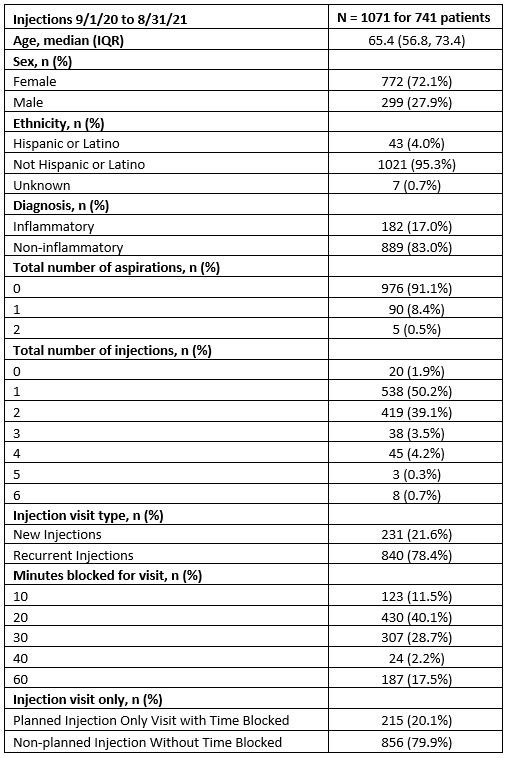
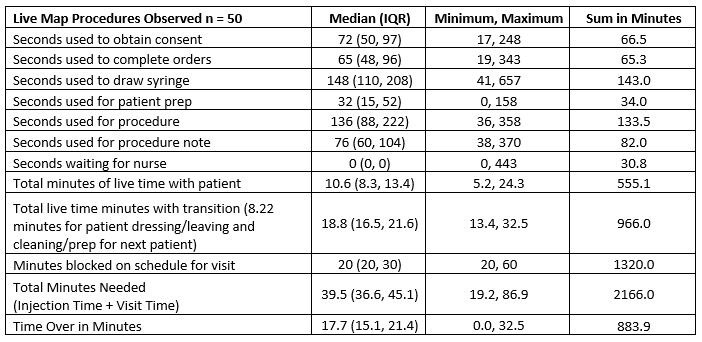
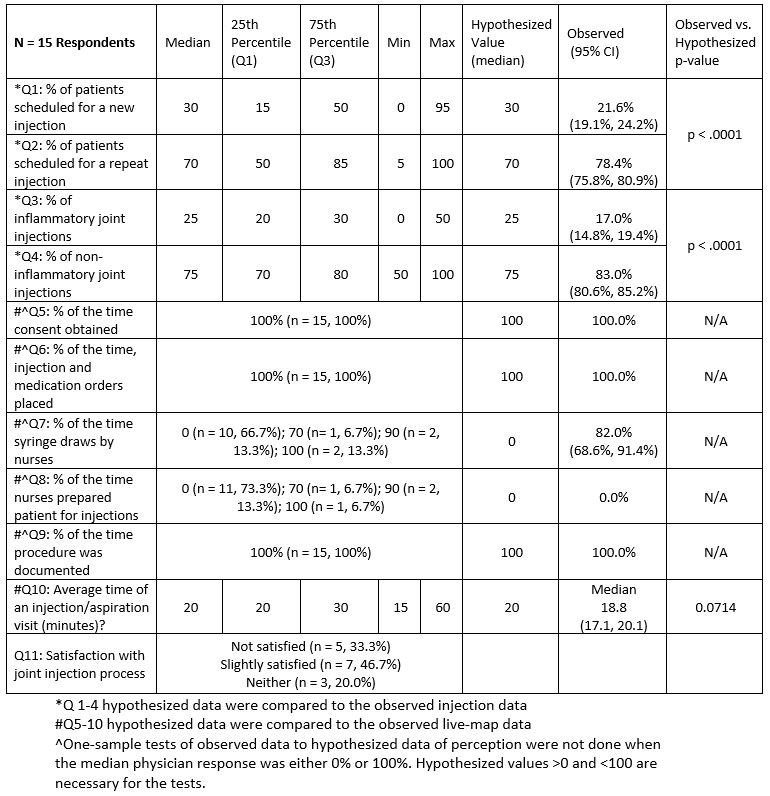
Methods: An 11-question survey was used to gauge physicians’ perception of the injection workflow and time allocation with 88% responses achieved. This was compared to observed live-mapping of 50 injections 9/7/2021-1/11/2022 and chart review of 1076 injections 9/1/2020 – 8/31/2021 extracted from the electronic health record. Patient demographics, disease and injection type, and time blocked for the procedure on the physician’s schedule were obtained. Observed proportions from chart review were compared to hypothesized proportions based on median responses to questions 1-9 by 1-sample proportion-tests. The median procedure time from live observation was compared to the median value of physician perception in question 10 by Wilcoxon signed-rank test.
Results: Our population consisted of 72% women and 28% men, median age of 65 years old, mainly non-Hispanic, receiving recurrent injections for non-inflammatory joint disease. Only 20% of the procedures had scheduled injection time versus (vs) 80% who didn’t per chart review (Table 1). Live-mapping data showed 8% of injections had scheduled time, while 92% were done as part of a standard clinic visit without blocked time, exceeding the scheduled clinic time by a median of 17.7 minutes (Table 2). Table 3 compares physician perception to observed chart review (questions 1-4) and live mapping (questions 5-10) patient injections. Physicians perceived doing 30% new/70% recurrent injections vs observed 21.6%/78.4% injections respectively (p< 0.0001). They perceived doing 25% inflammatory/75% non-inflammatory injections vs observed 17%/83% respectively (p< 0.0001). The perceived median time spent on an injection was 20 minutes vs observed median time 18.8 minutes (p=0.071). Physicians had 100% completion of consents/orders/documentation by both perception and observation. Nurses were perceived to assist with patient preparation 33% of the time and injection preparation 27% of the time but were observed to assist 100% and 82% of the time respectively. 80% of physicians reported low satisfaction with the process. We multiplied the number of unscheduled injections (856) by the median observed injection time (18.8 minutes) and divided it by physician full time equivalent (FTE 8.9) for this study resulting in an estimated 30 unblocked hours/clinical FTE/year over templated time as a result of unscheduled procedures at the current injection efficiency.
Conclusion: Time constraint is a common barrier to patient centered care and physician satisfaction. In our academic rheumatology center, the joint injection process took 17-19 minutes/injection. In addition, 80% of injections were done unscheduled resulting in an additional 30 clinical hours per physician per year over templated clinic time. 80% of physicians were not satisfied with the current injection process. Based on this data, we are redesigning the injection workflow to improve efficiency and physician experience.
To cite this abstract in AMA style:
Band M, Newman E, Berger A, Koons K, Duggirala M, Kuppuraju R, Nicholas III P, Bulbin D, Pugliese D, Cote J. Joint Injection Workflow in Rheumatology – an Opportunity to Improve Efficiency and Physician Satisfaction [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/joint-injection-workflow-in-rheumatology-an-opportunity-to-improve-efficiency-and-physician-satisfaction/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/joint-injection-workflow-in-rheumatology-an-opportunity-to-improve-efficiency-and-physician-satisfaction/