Session Information
Date: Tuesday, November 10, 2015
Title: Health Services Research Poster III: Patient Reported Outcomes, Patient Education and Preferences
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Discordance between patients with rheumatoid arthritis (RA) and their rheumatologists in their global assessments of disease activity affects around 33% of clinical encounters. The objective of this study was to understand the perspective of patients with measured discordance on issues like disease assessments and patient-provider communication.
Methods: We conducted individual interviews with 20 patients (six males and 20 females) with RA (ACR/EULAR 2010 criteria) who had patient-physician discordance as defined by a ≥25-mm absolute difference in global assessments of disease activity at the most recent rheumatology appointment within 4 weeks (median patient global assessment = 56 mm; median provider global assessment =15 mm). The interviews were audio recorded, transcribed verbatim, and checked for accuracy. Interviews were analyzed using content analysis by coding the texts, identifying themes and patterns and then grouping them into meaningful clusters. To aid interpretation of the qualitative data, the Clinical Disease Activity Index (CDAI) was collected from the most recent clinical evaluation, and participants also completed the pain visual analog scale (VAS) and the Patient Health Questionnaire-9 (PHQ-9).
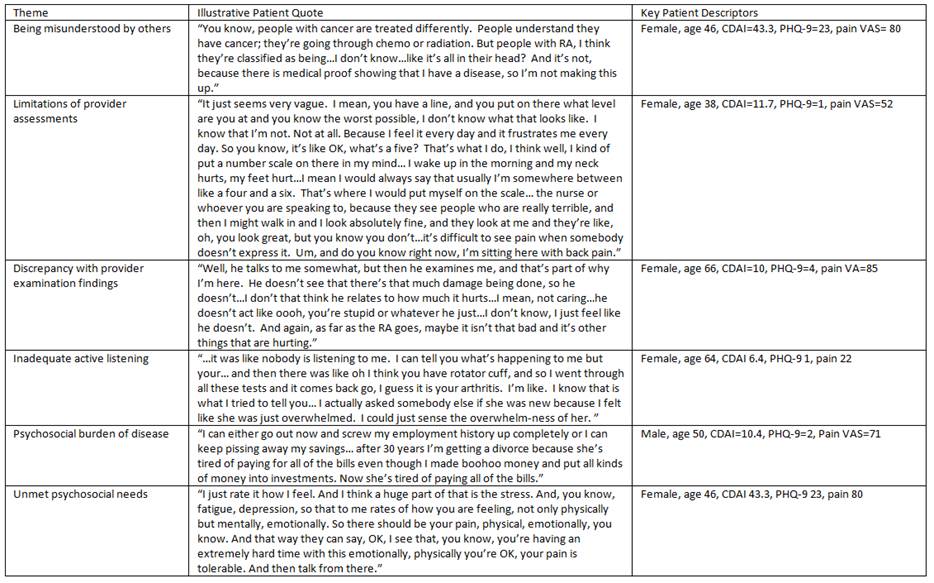
Results: The average age was 63 years (range 38-85). The medians (IQRs) for CDAI, pain VAS, and PHQ-9 were 10.2 (8.3 to 22.4), 61.5 (42.8 to 77.8), and 3.5 (2 to 7.8), respectively. Qualitative data analysis yielded six key themes (Table). Many patients described being misunderstood by others, including medical and non-medical communities, and distinguished their experiences from those with other, perhaps more objectively defined diseases. Not all patients reported feeling like their providers assessments differed from their own, but those who perceived discordance attributed it to providers’ failure to listen, lack of empathy, or rushed behaviors. Many reported consternation with completing pain, disability and global activity ratings, and few reported discussions of these with providers. Other patients did not necessarily understand the meaning of disease assessments (e.g., blood tests, x-rays). Patients also described the psychosocial burden of RA on daily life, noting unmet psychosocial needs and confusion about whether these issues should be addressed with their providers.
Conclusion: The findings of this study reveal several key themes for rheumatologists to take into account in their daily approach to patients with RA. The results should inform future studies aiming to enhance patient-physician communication and to develop management approaches targeting optimal health outcomes for patients with RA, including those that acknowledge the impact that RA has on daily living, which may not be currently perceived as important to disease assessments in clinic.
To cite this abstract in AMA style:
Davis JM III, Kvrgic Z, Plagge MM, Ridgeway JL, Asiedu GB. “It Was like No One Is Listening to Me”�: A Qualitative Study of the Lived Experiences of Patients with Rheumatoid Arthritis in the Setting of Patient-Physician Discordance in Assessments of Disease Activity [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/it-was-like-no-one-is-listening-to-me%ef%bf%bd-a-qualitative-study-of-the-lived-experiences-of-patients-with-rheumatoid-arthritis-in-the-setting-of-patient-physician-discordance-in-assessments-of-d/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/it-was-like-no-one-is-listening-to-me%ef%bf%bd-a-qualitative-study-of-the-lived-experiences-of-patients-with-rheumatoid-arthritis-in-the-setting-of-patient-physician-discordance-in-assessments-of-d/