Session Information
Date: Tuesday, November 14, 2023
Title: (2095–2140) RA – Diagnosis, Manifestations, and Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Diagnosis of a periprosthetic joint infection (PJI) in a patient with inflammatory arthritis (IA) is challenging, as features of IA flares can mimic an infection. We aimed to identify the optimal tests to diagnose a PJI accurately and efficiently in patients with IA.
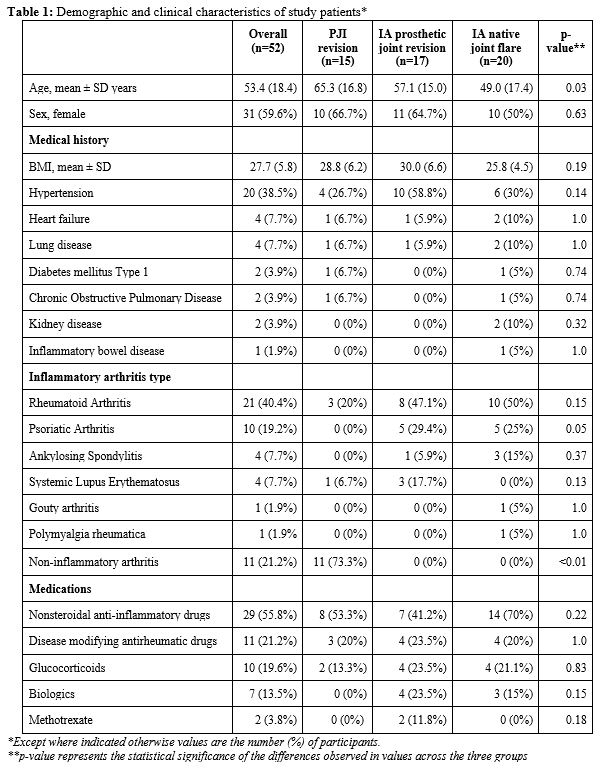
Methods: We included participants in three patient groups: 1) IA patients with a flaring native joint, 2) IA patients with a prosthetic joint undergoing aseptic revision, and 3) patients with PJI regardless of IA. Demographic characteristics were compared across the three groups. Blood and synovial fluid markers were compared across groups to assess the sensitivity and specificity in diagnosing PJI versus IA flares.
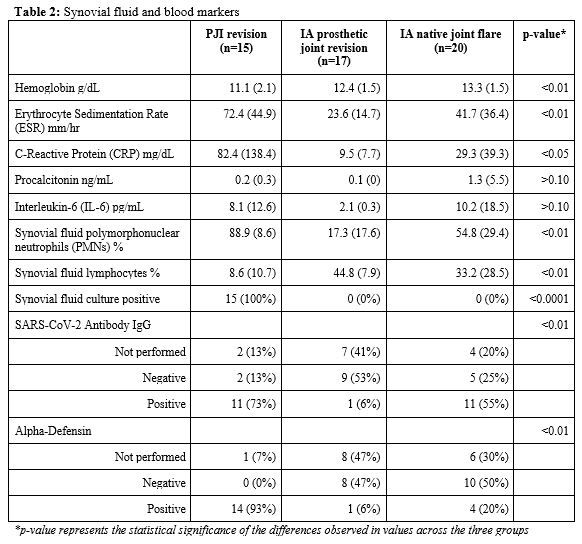
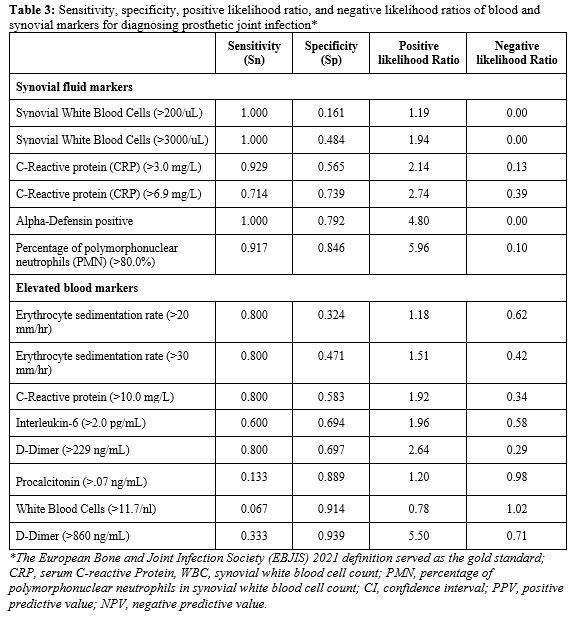
Results: This study included 52 participants, mostly female (60%), and 40% had rheumatoid arthritis. Among the three groups, the confirmed PJI patients were older (p=0.03), while no significant statistical differences were observed in the remaining demographic variables. Synovial fluid and blood markers were significantly different between groups. PJI cases had the highest average C-Reactive Protein (CRP) and there was a significant difference between the groups (PJI: 82 mg/dl, IA flares: 29 mg/dl, aseptic revisions:10 mg/dl, p< 0.05) (Table 2). Similarly, the percent of synovial fluid polymorphonuclear neutrophils (PMNs) was highest in PJI cases and significantly differed between groups (PJI: 88.9%, IA flares: 54%, aseptic revisions: 17%, p< 0.01). Among PJI cases, alpha-defensin was positive in 93%. However, positive alpha-defensin was also observed in 20% of flares and 6% of aseptic revisions, with a significant difference (p< 0.01). There was no significant difference in procalcitonin and IL-6 levels across groups. Synovial white blood cells (WBC) exceeding 3,000 cells/µL, positive alpha-defensin, CRP levels exceeding 3 mg/dl, and PMNs exceeding 80% were highly sensitivity but less specific in diagnosing PJI (Table 3). Synovial WBC counts exceeding 3,000 cells/µL, alpha-defensin positivity, CRP level exceeding 3 mg/dl, and PMNs exceeding 80% were highly sensitive yet less specific for PJI diagnosis. For example, while synovial WBC counts exceeding 3,000 cells/µL and positive alpha-defensin had 100% sensitivity for identifying PJI, their specificity was poor with 50% of IA native joint flares and 79% of aseptic revisions scoring positive for an infection, respectively. The relatively poor specificity of synovial WBC and alpha-defensin indicate that that there is a higher likelihood of these tests incorrectly detecting PJI in cases where it is not present. Positive tests for alpha-defensin or synovial fluid PMNs exceeding 80% increased the likelihood of diagnosing PJI by 5 and 6 times, respectively. However, in cases without PJI, a negative result for PMNs exceeding 80% only marginally increased the likelihood of accurately ruling out diagnosis by 1 time. IL-6, procalcitonin, and D-Dimer demonstrated high sensitivity and specificity, while ESR and CRP had 80% sensitivity but had significantly lower specificity.
Conclusion: Diagnosing PJI in patients with inflammatory arthritis remains challenging. Current efforts are examining whether next-generation sequencing may prove more effective than common clinical tests.
To cite this abstract in AMA style:
Goodman S, Mannstadt I, Tam K, Kochen A, Shakib L, Sculco P, Figgie M, Carli A, Miller A, Russell L, Nocon A, Donlin L. Is This Prosthetic Joint Infected or Flaring? [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/is-this-prosthetic-joint-infected-or-flaring/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-this-prosthetic-joint-infected-or-flaring/